Ultrasound-guided nerve blocks are becoming an integral aspect of multimodal pain management in emergency departments. Ultrasound guidance allows clinicians to visualize both the target structures (nerve and surrounding fascial planes) and the advancing block needle. In our experience teaching ultrasound-guided nerve blocks over the past 15 years, clear needle tip visualization is often the most difficult “microskill” to master. A misplaced needle can result in inadvertent vascular puncture or direct nerve injury. Here, we outline some practical techniques that allow learners to better visualize the needle tip during nerve blocks and improve success rates. These skills can elevate ultrasound-guided nerve blocks to become an essential element of your multimodal pain management of the acutely injured patient.
Explore This Issue
ACEP Now: Vol 40 – No 06 – June 2021Proper Equipment Setup
Ideal clinician and patient positioning improves success when performing any emergency department procedure. This holds true for ultrasound-guided nerve blocks. Unfortunately, patient positioning can be difficult in the acutely injured patient, adding another challenge. We recommend adhering to basic ergonomic principles to ensure that the view of the needle and ultrasound screen remain in the same line of sight when performing a block.1
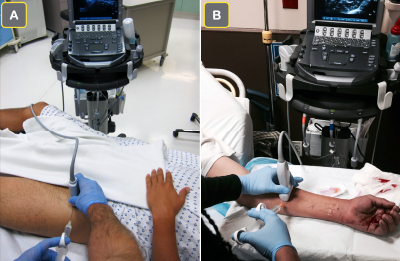
Figure 1A: The ultrasound screen is placed contralateral to the injured extremity when performing a femoral nerve block. This allows the clinician to view the ultrasound screen and the site of needle entry in the same line of sight.
Figure 1B: For a forearm nerve block for a palmar laceration, the ultrasound screen is placed on the ipsilateral side of the injury to allow for a clear line of sight.
photos: Arun Nagdev
The ultrasound screen positioning will vary depending on the block performed, but the general principle of keeping the ultrasound screen in line of sight is one of the keys to success. For example, when performing an ultrasound-guided femoral nerve block, we recommend placing the ultrasound screen contralateral to the site of injury (see Figure 1A). Conversely, for a patient with a palmar laceration (requiring a forearm nerve block), the clinician can place the ultrasound system on the same side as the injury to maintain clear line of sight (see Figure 1B). The clinician should determine the ideal position of both the patient and the ultrasound screen while setting up for the block. The extra few minutes spent up front determining the ideal ergonomic positioning will increase block success and often end up saving time overall.
Optimal Hand and Transducer Positioning
Optimal hand stability during ultrasound-guided nerve blocks can be accomplished with a few simple techniques. The operator should hold the ultrasound transducer with their nondominant hand and rest the medial aspect of their palm to stabilize the probe (termed “anchoring”) (see Figure 2A). The operator can also use their fourth or fifth finger to further stabilize the probe against the patient.
Pages: 1 2 3 4 | Single Page





No Responses to “Tips for Performing Ultrasound-Guided Nerve Blocks in the Emergency Department”