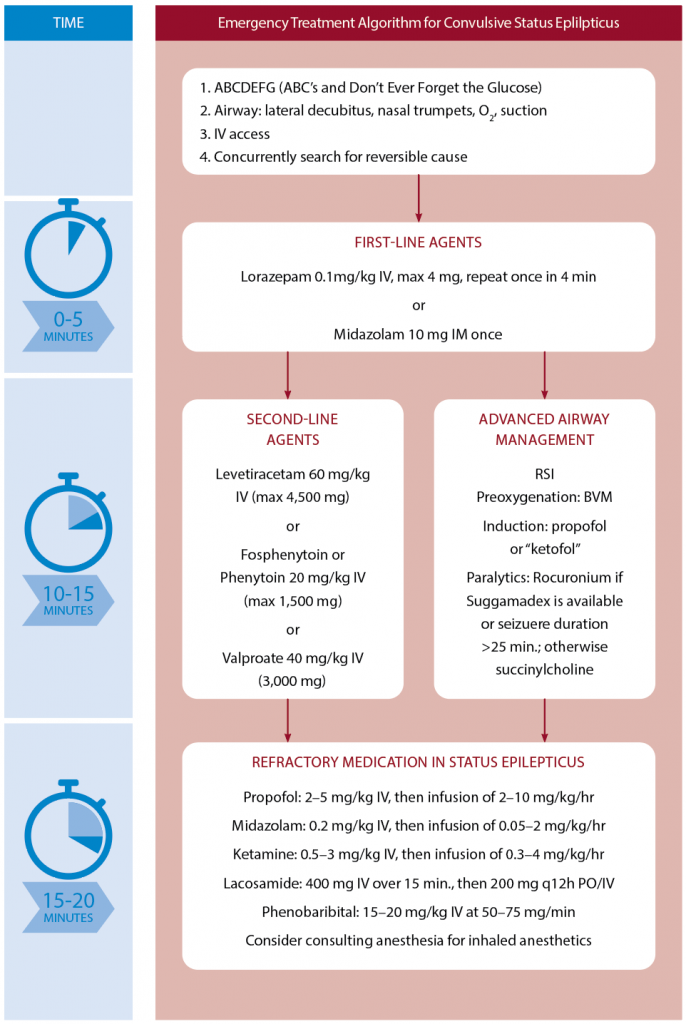
Second-Line Agents
After two adequate doses of IV lorazepam have been given two to four minutes apart, the drug you should reach for may surprise you. It’s propofol. Propofol should be considered concurrently with a traditional second-line agent such as levetiracetam, fosphenytoin, or valproic acid.9 It is important to understand that the goal of using propofol is to achieve seizure cessation, while the goal of traditional antiepileptic medications is to prevent seizure recurrence. Multiple trials have demonstrated unacceptable seizure durations of 30–45 minutes using traditional second-line agents without use of a sedative-hypnotic drug.10,11 Propofol use is familiar to emergency clinicians in other conditions and has been shown in recent meta-analysis to have a better disease control rate and faster results and reduced tracheal intubation time compared to barbiturates.12 The recommended dose is propofol IV bolus 2 mg/kg, followed by 50–80 mcg/kg/min (3–5 mg/kg/hr) infusion.
We should approach seizing patients in the emergency department swiftly and aggressively, with the goal of immediate seizure cessation.
Turning to intubation, some experts recommend ketofol (ketamine plus propofol) based on the theoretical benefit of blocking both N-methyl-D-aspartate and gamma-aminobutyric acid receptors with ketamine and propofol, respectively.13 I also recommend using a paralytic agent to maximize the chance of first-pass success. Long-term neuromuscular blockade should be avoided whenever possible so patients can be monitored for ongoing seizure activity and serial neurological exams can be conducted until EEG monitoring is available.
The choice of paralytic agent depends on patient factors, duration of seizure activity, and access to the rocuronium reversal agent sugammadex. If there are no clear contraindications for using succinylcholine and the patient has been seizing for less than 20–25 min, it is reasonable to use succinylcholine given its short duration of action. If sugammadex is available, consider rocuronium. Sugammadex should only be used in a controlled fashion to reverse the rocuronium after the airway has been secured and the patient has been stabilized. Its purpose in status epilepticus is only to reveal underlying physical seizure activity to aid in titrating sedative infusions rather than as a tool used for an anticipated difficult/challenging airway.
Choosing among antiepileptic drugs is less about any upsides and more about avoiding contraindications. The recent ESETT trial, which included adults and children with persistent benzodiazepine refractory generalized convulsive status epilepticus, found no difference between the use of levetiracetam, fosphenytoin, and valproate in seizure cessation and improved alertness by 60 minutes.14 However, phenytoin and fosphenytoin have sodium channel blockade effects, similar to the mechanism of action of certain toxidromes such as tricyclic antidepressant and cocaine overdose. The additional sodium channel blockade of phenytoin/fosphenytoin could therefore result in dangerous and even fatal cardiac dysrhythmias. These drugs should generally be avoided in toxicological causes of seizure for this reason. Although controversial, valproate should be avoided in pregnant patients.15 Perhaps the safest medication is levetiracetam dosed at 60 mg/kg IV (maximum 4.5 g).
Pages: 1 2 3 4 | Single Page






No Responses to “Tips for Managing Active Seizures in the Emergency Department”