
Explore This Issue
ACEP Now: Vol 37 – No 09 – September 2018Left: Day 1 – normal
Right: Week 3 – subtle periosteal reaction lateral aspect distal tibia
Case 3: occult distal radius fracture
The 69-year-old woman who fell on her outstretched hand: When she returned one week later, she was still tender and swollen and looked like she had a distal radius fracture. She was kept in a splint, and X-rays repeated at four weeks revealed the fracture.

Left: Day 1 – normal
Right: Week 4 – sclerosis across distal radius
Case 4: occult lateral tibial plateau fracture
The 72-year-old woman who twisted her knee: When she returned one week later, she was still unable to bear weight on the knee, and she was swollen and tender over the lateral joint line. Follow-up imaging revealed a lateral tibial plateau fracture.
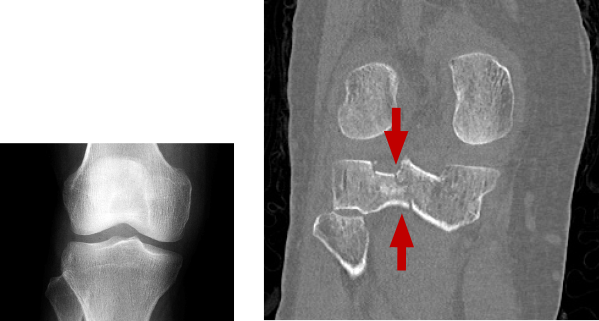
Left: Day 1 – normal
Right: Week 4 – sclerosis across distal radius
Our next column will deal with management strategies for suspected occult fractures in the emergency department.
 Dr. Sayal is a staff physician in the emergency department and fracture clinic at North York General Hospital in Toronto, Ontario; creator and director of CASTED ‘Hands-On’ Orthopedic Courses; and associate professor in the department of family and community medicine at the University of Toronto.
Dr. Sayal is a staff physician in the emergency department and fracture clinic at North York General Hospital in Toronto, Ontario; creator and director of CASTED ‘Hands-On’ Orthopedic Courses; and associate professor in the department of family and community medicine at the University of Toronto.
References
- Wheeless CR. Scaphoid frx: non diagnositic X-ray. Wheeless’ Textbook of Orthopaedics website. Accessed Aug. 17, 2017.
- Mallee WH, Wang J, Poolman RW, et al. Computed tomography versus magnetic resonance imaging versus bone scintigraphy for clinically suspected scaphoid fractures in patients with negative plain radiographs. Cochrane Database Syst Rev. 2015;(6):CD010023.
- Lin M. Beware the hidden tibia plateau fracture. Academic Life in Emergency Medicine website. Accessed Aug. 17, 2017.
- Mustonen AO, Koskinen SK, Kiuru MJ. Acute knee trauma: Analysis of multidetector computed tomography findings and comparison with conventional radiography. Acta Radiol. 2005;46(8):866-874.
- Likelihood ratios. Centre for Evidence-Based Medicine website. Accessed Aug. 17, 2017.
Pages: 1 2 3 4 | Single Page





No Responses to “Tips for Diagnosing Occult Fractures in the Emergency Department”