Imagine that on your next shift, you see two patients with hip pain and normal X-rays. Patient A is a 25-year-old male who fell down two stairs onto his right hip. He has a limp and lateral hip tenderness, but he has a good range of motion (neither shortened or externally rotated). His estimated pretest probability for a fracture is 10 percent.
Explore This Issue
ACEP Now: Vol 37 – No 09 – September 2018Patient B is a 78-year-old male who fell on his right hip from standing. He can’t walk due to the pain, is tender to palpation laterally at the hip, and has quite reduced active and passive range of motion of the hip due to pain (neither shortened or externally rotated). His estimated pretest probability for a fracture is 90 percent.
Again, both have normal X-rays of the hip and pelvis.
You mark Patient A’s 10 percent pretest probability of a fracture on a Fagan nomogram on the left axis, then draw a line from that mark through the estimated LR of 0.075 on the center axis and see where it intersects on post-test probability (ie, the right axis). See the blue line on Figure 1. Given the negative X-ray, you see the post-test probability of fracture is now less than 1 percent.
You do the same for Patient B, and despite his pretest probability of 90 percent for a fracture, you see the negative X-ray has driven the post-test probability of fracture down to around 40 percent. See the red line on Figure 1.
Negative X-rays in the face of a low pretest probability are unlikely to have a fracture, of course. However, we should keep the possibility of a fracture higher on the differential diagnosis for patients with a higher pretest probability for fracture and negative X-rays.
Remember this axiom: The purpose of any test is not to make the diagnosis but rather to affect our pre-test probability.
Case Resolutions
Case 1: occult mid-shaft clavicle fracture
The 12-year-old boy who fell on his shoulder: When he returned one week later he was still tender and swollen and looked like he had a clavicle fracture. He was kept in a sling, and X-rays repeated three weeks later revealed the fracture.
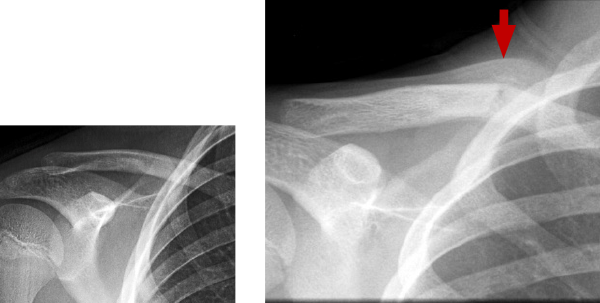
Left: Day 1 – normal
Right: Week 3 – fracture and callus
Case 2: occult distal tibia fracture
The 13-year-old girl with a twisted ankle: When she returned one week later, her mechanism was external rotation (a red flag, see image), and she was tender over her distal tibia. X-rays taken three weeks later showed an occult distal tibia fracture.
Pages: 1 2 3 4 | Single Page





No Responses to “Tips for Diagnosing Occult Fractures in the Emergency Department”