Three days later, the patient returned to the emergency department with severe foot pain and a cold, pulseless foot. Emergency vascular surgery was performed for a massive popliteal thrombosis; he never recovered full function of his right lower extremity.
Explore This Issue
ACEP Now: Vol 36 – No 05 – May 2017When to Suspect an Occult Knee Dislocation
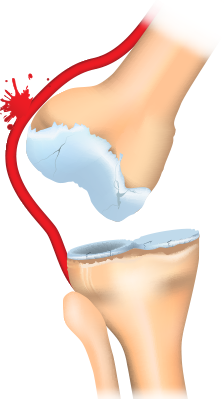
Anterior knee dislocation.
ILLUSTRATION: Chris Whissen & shutterstock.com
About 20 percent to 50 percent of all knee dislocations spontaneously reduce before patients arrive at the emergency department, and while patients may feel a shift of the knee joint, they may not recognize that their knee is dislocated. One pitfall in the history is assuming that a low-energy mechanism cannot cause a knee dislocation. A low-energy mechanism such as stepping off a curb in patients with a body mass index greater than 40 accounts for a significant proportion of missed occult knee dislocations. One study found that 47 percent of knee dislocations were due to low-energy trauma (eg, slips and falls), with 75 percent being in obese patients. Obese patients with low-energy trauma were more likely to have associated neurovascular injury than high-energy trauma patients in this cohort.
If patients have severe knee pain and a large effusion, check for a “loose knee.” Sometimes it is obvious that there is multidirectional ligamentous laxity when the examiner stabilizes the thigh and attempts to move the lower leg with the knee slightly flexed. A helpful rule of thumb is three of four knee ligament disruptions should be considered a knee dislocation until proven otherwise. Another clue: if patients complain of the knee buckling and are found to have a foot drop, then a knee dislocation should be suspected as the dislocation can cause a common peroneal nerve palsy. Lastly, upon lifting the patients’ legs by their heels, the dislocated knee may fall into hyperextension compared to the contralateral knee.
Workup of Suspected Knee Dislocation
The presence of normal distal pulses does not preclude occult popliteal artery injury as this has been shown to have a rate of 5 percent to 15 percent when normal pulses are present.
Ankle brachial index (ABI) and Doppler ultrasound imaging may miss small intimal injuries that clot after a few days. The gold standard is an arteriogram, but CT angiogram is more readily available.
Until recently, all patients with suspected knee dislocation underwent CT angiogram to assess for vascular injury. However, since the vast majority of patients who do have a vascular injury but have normal serial neurovascular exams and normal serial ABIs have intimal tears that do not require surgery, some experts recommend simply administering anticoagulants and admitting patients for observation without performing a CT angiogram.
Pages: 1 2 3 | Single Page





No Responses to “Tips for Emergency Physicians on Spotting Occult Knee Dislocation”