The Case
A 40-year-old man lost control while driving and collided into a barrier at 45 miles per hour. He was belted, no airbag was deployed, and there was no passenger intrusion. He did not lose consciousness and had full recollection of the event. He only complained of severe right knee pain.
Explore This Issue
ACEP Now: Vol 36 – No 05 – May 2017On examination, his primary survey was unremarkable. On secondary survey, there were no signs of head injury, but there was slight cervical spine tenderness without thoracic or lumbar spine tenderness. His chest and abdominal exams were normal. His focused assessment with sonography for trauma (FAST) exam was negative. His pelvis was stable. His extremity exam revealed a swollen tender right knee with an obvious effusion and very limited range of motion.
Discussion
One of the differential diagnoses that we don’t often think about is that of the occult knee injury. A cognitive forcing strategy should be employed every time we are confronted with a patient who presents to the emergency department with a significant knee injury but has a normal or near normal X-ray:
- Quadriceps tendon rupture
- Patella tendon rupture
- Lateral tibial plateau fracture
- Knee dislocation with spontaneous reduction
- Locked knee
- Compartment syndrome
Here, we will review some physical exam pearls to help improve our assessment of the knee and elucidate pitfalls in the diagnosis and management of one of the more serious but rare occult knee injuries. Spontaneously reduced occult knee dislocation is often missed and may result in ischemic complications culminating in limb amputation.
Knee Examinations in Patients with Severe Knee Pain
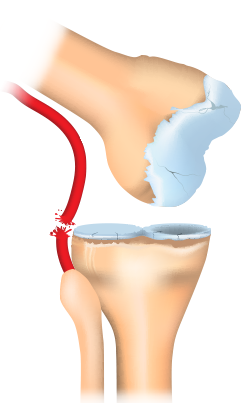
Posterior knee dislocation.
ILLUSTRATION: Chris Whissen & shutterstock.com
Many patients who have suffered an acute knee injury will experience pain that limits the physical exam. Clinicians may short-change their examination of the knee because they don’t want to cause more pain. Nonetheless, there are several tips to help patients relax enough to help facilitate provocative testing and the essential maneuvers. First, patients must be supine on a stretcher (not sitting in a chair), with both knees fully exposed. Place a pillow or roll under the distal femur so that the knee is relaxed at about 20 degrees of flexion to allow for provocative knee testing. If necessary, inject 3 mL of 1% lidoocaine into the knee joint before attempting provocative maneuvers.
The Case Continued
After placing a roll under the patient’s distal femur and injecting the knee joint with lidocaine, a full knee exam, including neurovascular examination of the lower extremity, was completed. This revealed normal pedal pulses bilaterally. However, there was significant ligamentous laxity of the knee. After the cervical spine was cleared and the patient was observed for six hours with serial examinations, he was placed in a full leg posterior splint and sent home with orthopedic follow-up.
Pages: 1 2 3 | Single Page





No Responses to “Tips for Emergency Physicians on Spotting Occult Knee Dislocation”