The patient was diagnosed with a Salter-Harris I fracture, placed in an air-stirrup, given crutches, and followed up in the minor fracture clinic on day eight. She had not been walking on it due to the pain.
Explore This Issue
ACEP Now: Vol 37 – No 02 – February 2018At follow-up, a little more detail on the mechanism of injury was obtained. She stated she was playing soccer on a muddy field and was wearing cleats. As she turned her body in to get away from another player, her foot remained stuck in the mud. In terms of mechanism, she was quite clear: Her body turned in with her foot stuck. This is external rotation of her ankle. Of note, the emergency physician had found her mildly sore at the distal fibular area and made the diagnosis of a Salter-Harris I fracture. Emergency department examination of the anterior joint line was not documented. When she came to the clinic, her pain was localized to the anterior joint line, as pictured in Case 3, Figure 3. Note the impressive swelling (better recognized when compared to the opposite side).

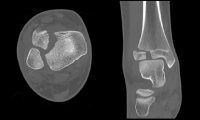
Case 3, Figure 4

Case 3, Figure 5
She was tender over the antero-lateral aspect of the distal tibia. She was non-tender over the lateral side along the fibula.
In reviewing the X-rays (Case 3, Figure 4, cropped) and now knowing where her pain localizes, it may be easier to detect the abnormality: a Salter-Harris III fracture of the distal tibial epiphysis, a Tillaux fracture.
Case 3, Figure 6
On the anterior-posterior and mortise views, a displaced intra-articular fracture is seen (Case 3, Figure 5, arrows). On the lateral view, it is subtle, but the fragment is mildly anteriorly displaced (Case 3, Figure 5, arrow).
This is a displaced intra-articular fracture. A CT scan confirmed the position. The patient underwent surgery the following day (see CT in Case 3, Figure 6, and intraoperative picture in Case 3, Figure 2).
A Tillaux fracture occurs in girls about 11–14 years old and boys about 12–15 years old because the distal tibial growth plate starts to fuse around these ages. It fuses from the medial half across to the lateral side. With external rotation, the syndesmosis (anterior distal tibiofibular ligament) is stressed, and the force separates the open (lateral) part of growth plate. When the force hits the closed part of the growth plate, the force exits down into the joint.8 The result is a Salter-Harris III fracture. This is the Tillaux fracture. Of note, a related injury exists, a Salter-Harris IV fracture. This has the same mechanism and involves the same age groups, but a triplane fracture can be seen on the lateral view to extend posteriorly up the distal tibial metaphysis.
Summary
These three injuries are uncommon but commonly missed. They serve to highlight the importance of mechanism and anterior joint line tenderness of the ankle. The clinical clues to these uncommon diagnoses are often present, but they can easily escape detection.




2 Responses to “Tips for Catching Commonly Missed Ankle Injuries”
March 3, 2018
abwExcellent article. Thank you.
July 30, 2018
Arun SayalThanks abw!
Happy to share these earls from our orthopedic surgeons – and from our patients.
Thanks to both groups for teaching me!
Arun