For nearly two years, ACEP has been fighting to ensure that the federal government’s implementation of the No Surprises Act has been in accordance with Congressional intent. Using every channel available on the federal, state, regulatory and legal channels, we have pushed for comprehensive policy and the fair implementation of those policies. Despite our gains on the policy side, the implementation of the law continues to be problematic.
Explore This Issue
ACEP Now: Vol 42 – No 06 – June 2023We’re pushing to fix the flawed implementation on several fronts. From a legal perspective, we have asked the courts to stop the unlawful requirement by the Departments of Health and Human Services, Labor, and Treasury (the Departments) that forces arbiters during the federal independent dispute resolution (IDR) process to illegally emphasize the qualifying payment amount (the QPA, or the median contracted amount) over other factors listed in the statute (patient acuity and complexity; training and experience of the provider; market share of provider/health plan; teaching status and case mix of facility; and previous experience attempting to enter into contractual agreements).
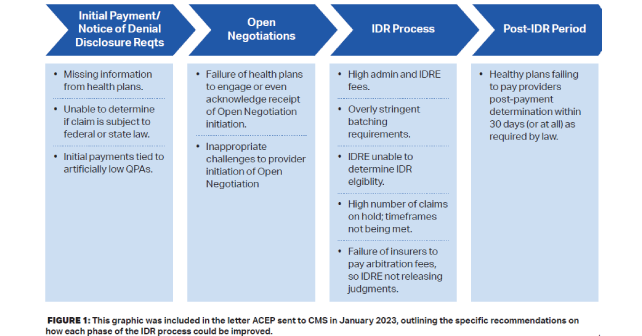
On the regulatory front, our team is pressing HHS to implement and enforce the policy the way it was written. We’re also pressing CMS to: 1) address its excessive increase of the IDR fees; 2) modify the flawed policy that allows limited batching of claims; 3) require more transparency around the calculation of the QPA; and 4) improve its enforcement over health plans that are skirting numerous requirements—most notably not providing the required information that identifies whether a claim is subject to the federal IDR process and not paying physicians what they owe after an arbitration in which the physicians win.
Finally, on the legislative side, we are working with our Congressional allies to put pressure on the Administration to address these significant implementation issues.
Much has happened since the No Surprises Act moved into the implementation phase, so let’s walk through the timeline of key events.
December 2021
ACEP, along with the American Society of Anesthesiologists and the American College of Radiology, filed a lawsuit against the government in Illinois in December 2021, arguing that the second Interim Final Regulation (Final Reg) implementing the No Surprises Act was fatally flawed and should be vacated. The Interim Final Reg set the QPA as the presumptive payment amount for out-of-network services during the IDR process. The Texas Medical Association (TMA) and other plaintiffs filed a similar suit in the Eastern District of Texas, and in early 2022, the court ruled in favor of those plaintiffs, vacating the Interim Final Reg nationwide. ACEP then withdrew its lawsuit and joined other societies in filing amicus briefs in support of the TMA case.
Pages: 1 2 3 | Single Page





No Responses to “The Surprise Billing Fight Continues”