A few years ago, emergency department leaders were given a valuable gift. The Joint Commission and then the Centers for Medicare & Medicaid Services (CMS) identified hospitals reducing the boarding of admitted patients as a priority for safety and quality of care. This was an opportunity to bend the curve on the amount of time patients spent in the ED, a curve that had been on an upward trajectory for years in many hospitals. This time interval, referred to in the ED literature as “boarding time,” requires management by ED leaders and hospital administrators. Both groups promoted measures with The Joint Commission that reduced boarding time. They wrote standards that emphasized the importance of ED flow to minimize ED boarding.
Explore This Issue
ACEP Now: Vol 34 – No 12 – December 2015Then in 2011, CMS published a set of performance measures that highlighted the ED. “ED-1, Admit Decision Time to ED Departure Time for Admitted Patients” was an important measure. The CMS defined the measure in a positive fashion: median time from admit decision time to time of departure from the emergency department for emergency department patients admitted to inpatient status. The rationale for this measure was the opportunity for emergency physicians to influence behavior by hospital administration and the admitting medical staff of the hospital. As the measure states, “Reducing the time patients remain in the emergency department can improve access to treatment and increase quality of care. Reducing this time potentially improves access to care specific to the patient condition and increases the capability to provide additional treatment.”
The measure was implemented in 2012 and was subject to public reporting in 2013. The simple definition and explanatory language became a very complicated process for many hospitals. The challenge was to define “admit decision time.” The Emergency Department Benchmarking Alliance (EDBA) asked its 1,100 ED leaders to describe the time marker that had been implemented in their hospital. The reported definitions included actions by the ED clerk (placing a bed order), the ED charge nurse (contacting the bed coordinator), the admitting physician (writing an admission order), and the emergency physician (changing status to admitted in the ED information system). From the hundreds of answers to this question, it was apparent that there were wide variations in the definition of this time stamp.
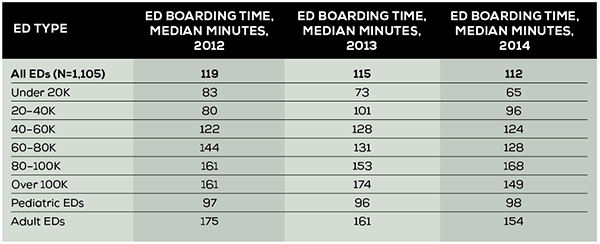
The EDBA initiated collection of the performance measure in 2012. Unlike CMS, which reports all EDs as one group, the EDBA reports the measure by cohorts. The median ED boarding times for the years 2012, 2013, and 2014 are summarized in Table 1. Reporting the data by cohort gives ED leaders a much more precise comparison based on ED volume and patient population served. The highest number is found in adult EDs and those EDs seeing between 80,000 and 100,000 patients per year. These EDs have boarding times of around 160 minutes. The low-volume EDs, seeing fewer than 20,000 patients, have boarding times that average 65 minutes, nearly a 100-minute difference. The boarding time median of 119 minutes in 2012 has been decreased to 112 minutes in 2014.
But in many EDs, and in particular those in the 20,000 to 60,000 cohorts, the boarding time has actually increased over the three years measured. There is clearly an opportunity gifted from CMS and The Joint Commission to allow ED leaders the traction needed to negotiate better hospital flow for admitted patients. More ED physicians and nurses need to engage in the efficient processing of patients needing inpatient services. In most hospitals, this will primarily be focused on patients being admitted to the same hospital, which on average is 17 percent of overall ED volume. But processes will also facilitate the movement of patients to admission units of other hospitals when transfers are necessary, which is about 2 percent of patients in the average ED.
Boarding of inpatients in the ED leads to crowded conditions, lack of patient care areas, insufficient staff to process all ED arrivals, and then a deadly cascade. The cascade will typically include prolonged patient waiting times, increased suffering for those waiting for service, unpleasant treatment environments, ambulance diversion, and poor patient outcomes. The cascade then leads to dissatisfied ED staff, frustration, and turnover at all levels. Overwhelmed EDs also lack the capacity to respond to community emergencies and disasters.
The timely processing of patients who are admitted to the hospital or transferred for admission to another hospital improves the overall flow rate of all ED patients. This leads to a culture of timeliness and satisfaction for all patients who arrive for ED service and reduces walkaway rates.
Where have EDs had success in improving admission flow? Primary work is done outside of the ED, with the global recognition that reduced boarding times are associated with reduced overall hospital length of stay, improved quality of care, and closer adherence to established hospital pathways. ED nursing leadership needs to focus its efforts on the nursing administration to link rapid flow of inpatients to nursing incentives. These may be financial (credit for nurse worked hours going to the inpatient unit rather than the ED), communication enhancement (timesaving patient turnover methods from ED to inpatient nurses), and/or recognition (award programs for competing nursing units).
On the physician side, most EDs now admit the majority of patients to hospitalists or group practices, including resident teams. The emergency physicians have the opportunity to negotiate with those services regarding the elements of improved patient service and pathway compliance. Many admitting physicians want a patient to be completely “worked up” by the time that patient will reach the floor and have the most important therapies started. The emergency physician can offer those elements if the admitting service will provide a timely response to emergency physician calls, a rapid concordance on the need for admission, and the timely delivery of an “order to admit.” The emergency physician also needs to facilitate the work of the admitting physician with an organized and complete history and physical exam on the patient record and transition-of-care communication that is clear and concise.
The work of the emergency physicians and nurses together will lead to a process of effective care and communications and then reduce blocking behaviors by staff in the admitting areas of the hospital.
There are a growing number of sources to use for best practices in the admission process. It is the opportunity to use them to bend the curve of boarding time that will improve the care and service of all ED patients.
Pages: 1 2 3 | Multi-Page





No Responses to “Reducing Boarding Time in the Emergency Department Can Improve Patient Care”