
Of note, most successful educational interventions were less than one hour long, suggesting that improvements are attainable even with time constraints. An important aspect of educational interventions is a focus on warning signs and symptoms that should alert emergency physicians to further investigate whether the patient may be a victim of trafficking. Examples of these warning signs include inconsistencies in one’s explanation of an injury, accompanying person speaking on behalf of the patient, signs of physical or sexual abuse, medical neglect, untreated sexually transmitted infections and/or excessively anxious behavior.13 These trainings should also emphasize the importance and application of trauma-informed care.
Once emergency staff has a foundational understanding of sex trafficking, the next step is to implement a standardized screening tool. Emergency physicians and nurses should utilize a screening tool any time they have a reason to suspect a patient may be in a trafficking situation; an understanding of potential warning signs is key as these red flags will alert the clinician to proceed with a formal screening. Importantly, the threshold for suspicion should be kept low to reduce the likelihood of missing a case of trafficking. Many screening tools exist, although they vary considerably in length and design. To date, two screening tools have been validated for use in the emergency department setting.
The Greenbaum Tool was developed specifically for use in pediatric emergency departments in patients between the ages 13 and 17.14
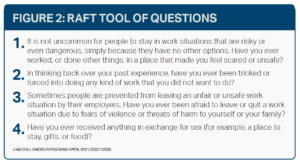
Rapid Appraisal for Trafficking (RAFT) tool was validated in 2021 for use in the adult ED patient population and is a comprehensive trafficking screening tool for use in health care settings.15 These screening questionnaires should be readily available to ED staff—either at the nurses’ station or embedded in the electronic medical record—or should be memorized and rehearsed for faster recall.
Setting Protocols in Place
When faced with a positive screen, ED staff may be unsure of how to best assist their patient. Thus, another crucial step to improve the care of trafficking victims is the implementation of standardized protocols. These protocols should integrate a screening tool with guidelines for the next steps to assist the victim. The HEAL Trafficking and Hope for Justice’s Protocol Toolkit is a great starting place for health care institutions to develop their own protocols.16 When developing a protocol, it is necessary to identify local organizations and services that can assist victims as the patient may have many immediate needs that need to be addressed including housing, medical follow-up, mental health services and substance use treatment. Moreover, these protocols will provide procedures to ensure the safety of the patient and staff as well as guidelines on when to involve outside agencies, such as local, state, and federal law enforcement and child protective services.
Pages: 1 2 3 4 | Single Page



No Responses to “Recognizing Human Trafficking Victims as Patients in the ED”