- Norepinephrine (Levophed). Norepinephrine has become the go-to pressor for nearly all types of shock for several reasons. Unsurprisingly, it is also a fantastic push-dose pressor.4 It has more a1 than b1, so most of the blood pressure effect is from peripheral vasoconstriction. Although it has some b1 to support patients with myocardial depression, it doesn’t tend to have as much arrhythmogenic effect as epinephrine, making it a great balanced pressor. Because norepinephrine has been widely adopted as the go-to pressor in the ED, infusion bags are generally readily available, and the enterprising emergency physician can draw a bolus dose directly from the bag (which will helpfully be labeled with the concentration). Dosing is similar to epinephrine, 10-20 micrograms every three to five minutes.
Although norepinephrine hasn’t historically had the same popularity as phenylephrine and epinephrine in the ED, I have found myself using it more often because of its balanced side-effect profile and easy availability.
Explore This Issue
ACEP Now: June 2025 (Digital)- Vasopressin (“Vaso”). Vasopressin is a non-catecholamine vasopressor, acting primarily on the V1 Because of its unique mechanism of action, it provides vasoconstriction but is generally less dependent on pH and may spare some of the pulmonary artery constriction seen with phenylephrine, a feature potentially desirable for patients with right heart decompensation or pulmonary hypertension. Use in the ED has mainly been described in case reports.5 Dosing is typically 0.4 to one unit once.
Perils and Pitfalls
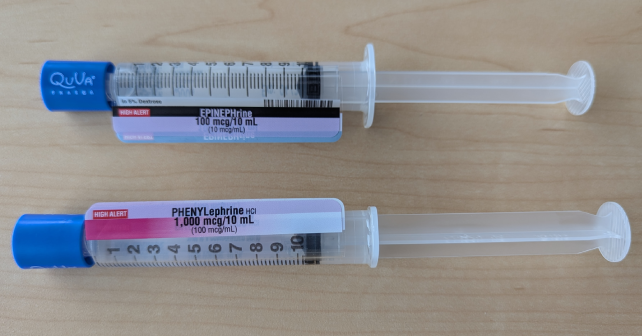
Now that we have reviewed the common push-dose pressors and their dosing, what are the common perils and pitfalls? The most common, by far, is dosing. There have been a number of reports suggesting orders-of-magnitude errors; these tend to almost invariably result in overdoses.1,6-8 Multiple sources will describe how to mix up push-dose pressors yourself.9-11 For example, to make push-dose epinephrine from the code cart dose, you take the 1 mg in 10 mL syringe (1000 mcg in 10 mL = 100 mcg per mL), remove 1 mL (100 mcg) and then mix it into 9 mL of a saline flush, giving a final 10 mcg/mL concentration. However, that math is tricky even when you are relaxed, and mixing this under a high-stress, high-stakes scenario is a recipe for mistakes.12 Instead, I suggest you work with the pharmacy to stock pre-made syringes and have them readily available.1 These have the convenience of being compounded ahead of time and will have standardized concentrations.
Otherwise, the most common errors I have seen are trying to use a push-dose pressor when a continuous vasopressor is needed, and failing to diagnose or treat the underlying cause of the hypotension. If you intubate a profoundly hypotensive patient with propofol, no amount of push-dose pressor will be superior to resuscitating beforehand! Like peripheral administration of vasopressors, peripheral administration of push-dose pressors is safe; when administered into a large bore, well-functioning IV catheter, the risk of extravasation is minimal.9,13,14
Pages: 1 2 3 | Single Page





2 Responses to “Push-Dose Pressors in the Emergency Department”
July 7, 2025
Seattle ER docGreat column. I’d love to see a follow up: what is the evidence that push dose pressors make a difference in patient outcomes?
We could just be treating numbers on a monitor, or maybe it’s actually helping the patient. Is there value in certain situations (e.g. EMS transport, bridging to pressor infusion in septic shock) but not in other situations (e.g. transient hypotension after intubation or procedural sedation)? A deep dive into the topic would be great.
December 29, 2025
Craig ButtonAs a nurse educator I really cringe when I see flushes being used to mix any medication. To many of the creators/influencers etc. have people mixing in a flush that is actually labeled for flush only and then they say label but don’t actual say what’s on the label.
The concept of push dose has been around for 25+ years. Was using it in SICU and in the OR forever it seems.