Welcome to Critical Care Time, a new critical care-focused column from ACEP Now.
Explore This Issue
ACEP Now: June 2025 (Digital)My goal in this column is to share tips, tricks, and emerging concepts from the intensive care unit (ICU) that you can use on your next shift in the emergency department (ED). Whether you are acutely resuscitating a critically ill patient or managing a boarding ICU patient, my goal is to give you practical knowledge from critical care-trained emergency physicians who know what it is like to work in the ED.
If there are topics that you want me to cover, don’t hesitate to reach out. This column is for you!
For this inaugural column, I wanted to start with a topic near and dear to my heart: push-dose vasopressors in the ED. I know I am not the only one to have my stomach drop while listening to the blood pressure cuff cycle again and again before displaying a number far lower than what I was hoping for. Mastering the use of push-dose pressors ensures that feeling is short-lived by giving you tools to rapidly and appropriately manage sudden hypotension.
What is a Push-Dose Pressor?
To keep it simple, a push-dose pressor is any vasopressor administered as an IV push—essentially, a bolus of pressor.1 Push-dose pressors can come in handy in three situations:
- Anticipated transient hypotension. Perhaps you have decided to perform procedural sedation with propofol, a known vasodilator. Having a push-dose pressor at the ready will ensure that you can counteract any transient hypotension that occurs after administration of the medication. Anesthesiologists do this all the time after bolusing propofol for induction of anesthesia.
- Known hypotension, as a bridge to a continuous infusion of a pressor. Your patient is sick and already severely hypotensive, but you are waiting for a nurse to obtain a pressor from the pharmacy, or for your pharmacist to compound the bag. Using push-dose pressors can be your lifeline while waiting for the infusion bag to arrive.
- Unanticipated hypotension. Finally, you may find yourself in an unexpected situation where you need a pressor immediately, but do not have any readily available in your location. You can use medications found in the crash cart to quickly create a push-dose pressor.
Common Vasopressors
So, what pressor do you use? Let’s review the most common:
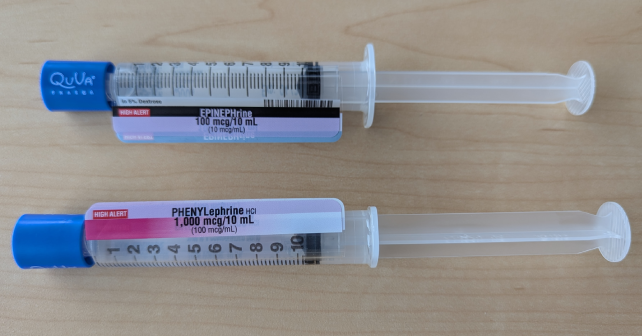
- Phenylephrine (Neo-Synephrine or “Neo”). Phenylephrine is the prototypical push-dose pressor and is classically given by anesthesiologists after induction. A pure a1– agonist, phenylephrine gives you peripheral vasoconstriction but no increase in cardiac output. Perfect for someone who has vasodilated or in need of increased afterload, phenylephrine is a great choice for unstable atrial fibrillation with rapid ventricular response or after a bolus of propofol. However, because it does not give you any increase in cardiac output, it isn’t an optimal choice for someone with myocardial depression. Typical dosing of phenylephrine is 50-200 micrograms every three to five minutes. (When a patient is acutely unstable, I set the blood pressure cuff to cycle every three to five minutes. This way, you can give another dose with each cycle of the cuff!)
- Epinephrine (“epi”). Epinephrine has more balanced a1 and b Because of this, it will give you both peripheral vasoconstriction from the a1 and an increase in heart rate (chronotropy) and contractility (inotropy) from the b1. However, because of the b1 effect, tachydysrhythmias are a common side effect.2 Epinephrine has the advantage of being easily accessible in most locations of the hospital, as it is stocked in code carts. Because of its availability, it has become the push-dose pressor of choice for many emergency physicians and for critical care transport.3 Typical dosing of epinephrine is 10-20 micrograms every three to five minutes.
Alternative Vasopressors
Phenylephrine and epinephrine are the most common push-dose pressors used in the ED. However, emerging evidence also suggests alternative agents as options.
Pages: 1 2 3 | Single Page






2 Responses to “Push-Dose Pressors in the Emergency Department”
July 7, 2025
Seattle ER docGreat column. I’d love to see a follow up: what is the evidence that push dose pressors make a difference in patient outcomes?
We could just be treating numbers on a monitor, or maybe it’s actually helping the patient. Is there value in certain situations (e.g. EMS transport, bridging to pressor infusion in septic shock) but not in other situations (e.g. transient hypotension after intubation or procedural sedation)? A deep dive into the topic would be great.
December 29, 2025
Craig ButtonAs a nurse educator I really cringe when I see flushes being used to mix any medication. To many of the creators/influencers etc. have people mixing in a flush that is actually labeled for flush only and then they say label but don’t actual say what’s on the label.
The concept of push dose has been around for 25+ years. Was using it in SICU and in the OR forever it seems.