Drug overdoses are a leading cause of accidental death in the United States, representing a persistent and escalating health crisis. According to recent data from the Centers for Disease Control and Prevention (CDC), overdose deaths have exceeded 100,000 annually since 2021, with approximately 75 percent involving opioids—a proportion that continues to rise.1
Explore This Issue
ACEP Now: June 2025 (Digital)Even in nonfatal opioid overdose cases, there is a significant increase in both short- and long-term mortality. One study found a 5.5 percent mortality rate within one year among patients discharged from the emergency department (ED) following a nonfatal opioid overdose. Alarmingly, more than 20 percent of those deaths occurred within one month, and 4.6 percent occurred within just two days of discharge.2 Another study revealed that patients who improved with naloxone after a nonfatal opioid overdose had a 13-fold increase in mortality within one year.3 These numbers underscore the impact of timely and effective intervention—both in the acute moments after an overdose, and in the days to months following ED discharge.
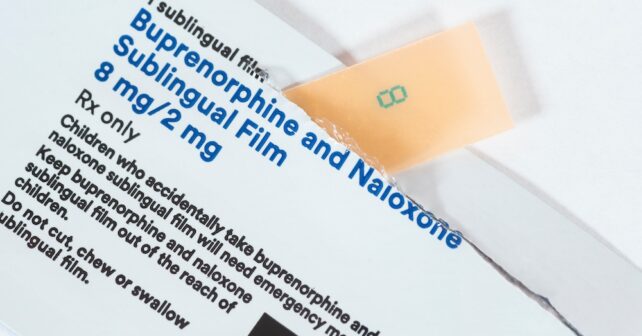
Buprenorphine, a partial opioid agonist approved for the treatment of opioid use disorder (OUD) by the U.S. Food and Drug Administration in 2002, is a cornerstone of evidence-based care for managing OUD. It effectively reduces cravings and withdrawal symptoms with minimal adverse effects. It is also proven to improve engagement in addiction treatment when compared to referral alone.4 These benefits translate into reductions in all-cause and opioid-related mortality.5,6
Prehospital Bupe
Emergency medical services (EMS) often serve as the first point of contact with the health care system for many individuals experiencing overdose or withdrawal. The CDC reported that between January 2018 and March 2022, the rate of EMS responses for nonfatal opioid overdoses nearly doubled, from 98.1 to 179.1 per 10,000 EMS calls.7 Moreover, research has shown that nearly half of all individuals who suffer a fatal overdose had at least one EMS encounter in the preceding year.8,9 It is clear these encounters are critical moments for potential intervention.
Across the country, a growing number of EMS systems recognize and embrace this opportunity to bring lifesaving and symptom-improving treatment to patients before they reach the hospital.10,11 Paramedics—and, in some places, even EMTs—are being trained to assess patients for buprenorphine eligibility and administer the medication in the prehospital setting. This is particularly important because studies have found that up to 47 percent of patients decline EMS transport to the hospital after being revived from an overdose.12,13,14 For these individuals, the brief EMS encounter could be their sole interaction with the health care system. It may be their only chance to initiate OUD treatment, receive counseling, and get connected to follow-up care.
Pages: 1 2 3 | Single Page





No Responses to “Prehospital Buprenorphine Is a Powerful Tool in the Opioid-Crisis Fight”