
A 47-year-old male with a medical history of hypertension, and, prior left upper lobe Pancoast tumor status, post video-assisted left upper lobectomy with chest wall and ribs 1-3 resection, presented to the emergency department (ED) with dyspnea, chest heaviness, and near syncope. He was found to be diaphoretic, speaking two- to three-word sentences, tachycardic to 150 bpm, and episodically hypotensive, with oxygen saturations in the 70 percent range on room air.
Explore This Issue
ACEP Now: Feb Digital 01-DLimited point-of-care ultrasound (POCUS) demonstrated a pericardial effusion and a large left-sided pleural effusion. The heart was inferiorly displaced; the apical four-chamber view was obtainable with the probe positioned superior to the umbilicus. Evidence of cardiac tamponade was present, including right ventricular diastolic collapse and greater than 25 percent mitral valve inflow velocity variation (see figure 1). Thoracic surgery requested CT imaging to evaluate for surgical complication; however, the patient was too unstable.
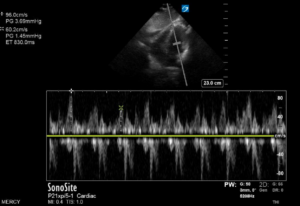
Figure 1. (A) Mitral valve inflow (MVI) velocity variation measured prior to chest thoracostomy. In this patient, MVI velocity variation is elevated at 37.5 percent, which is indicative of tamponade physiology. (B) Normalized MVI velocity variation after chest tube thoracostomy.
Under ultrasound guidance, a left tube thoracostomy was placed with evacuation of approximately two liters of serosanguinous fluid, resulting in marked improvement and near complete correction of abnormal vitals. A repeat bedside ECG showed complete resolution of tamponade findings (Figure 2), no appreciable pericardial effusion, and relocation of the heart to typical anatomic location.
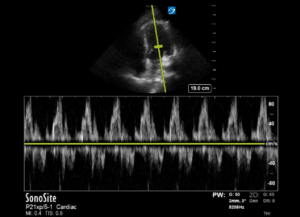
Figure 2. (A) Collapsible right heart and signs of tamponade with small pericardial effusion seen at patient presentation and (B) resolution of tamponade findings after chest thoracostomy was performed.
Diagnosis and Management
Tension physiology is the result of external cardiac compression caused by air, fluid, or a mass when they grow or accumulate rapidly or to a sufficient size to cause localized displacement of structures or changes in pressure dynamics. Compression of the vena cava reduces preload, while compression of the right heart impairs cardiac filling, reducing stroke volume and precipitating obstructive shock.
In normal physiology, inspiration leads to increased negative intrathoracic pressure, allowing for increased preload of both ventricles. In tamponade, there is increased interventricular dependence, and the septum bows more dramatically into the left ventricle during inspiration, decreasing the amount of blood filling the left heart. This is measured with sonography by placing the pulse wave Doppler gate in the left ventricular space at the opening of the mitral valve leaflets in an apical four chamber view, thereby measuring the speed of left ventricular filling. Mitral valve inflow velocity variability greater than 25 percent is characteristic of cardiac tamponade, as natural interventricular dependence throughout the respiratory cycle is increased and can be thought of as the sonographic equivalent of pulsus paradoxus.1
Pages: 1 2 3 | Single Page





No Responses to “POCUS-Guided Management of Tension Hydrothorax Causing Cardiac Tamponade”