Case Vignette
An unresponsive, unknown male around 50 years old presents to the ED via EMS post-return of spontaneous circulation (ROSC) after being found in pulseless electrical activity (PEA) cardiac arrest. Current vitals include a heart rate of 85 bpm, blood pressure of 78/40 mmHg, and oxygen saturation of 86 percent with bag-valve-mask assisted ventilations. The team is discussing how to rapidly optimize hemodynamics to intubate as soon as possible.
Explore This Issue
ACEP Now: February 2026 (Digital)When?
Push-dose epinephrine (EPI) and phenylephrine (PHE) can be very effective to augment poor hemodynamics in a variety of clinical situations in the ED including procedural sedation, peri-intubation hypotension, shock syndromes, or as a bridge to continuous vasopressor infusions (CVI).
Why?
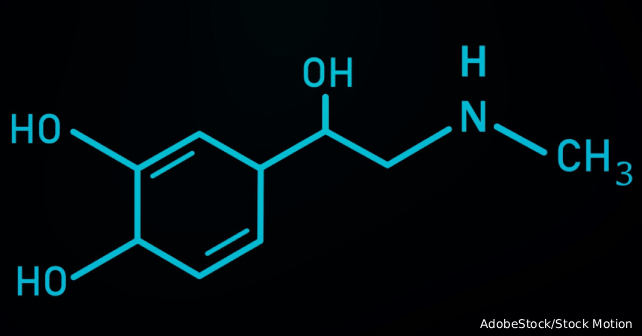
Phenylephrine works as an α1 agonist causing systemic vasoconstriction, whereas epinephrine is an α1, β1, and β2 agonist producing increased chronotropy and inotropy in addition to vasoconstriction. Push-dose PHE and EPI allow for rapid, but temporary, improvements in hemodynamics given their quick onset and short duration.
How?
Phenylephrine
- Dose: 50-200 mcg every 2-5 minutes
- Onset: 1 minute
- Duration: 15 minutes
- Warnings/Precautions: May cause reflex bradycardia and hypertension. Caution the variety of concentrations in pre-made syringes as they usually vary from 50-100 mcg/mL.
Epinephrine
- Dose: 5-20 mcg every 2-5 minutes
- Onset: 1 minute
- Duration: 5 minutes
- Warnings/Precautions: May cause tachycardia and hypertension. Caution should be used to ensure the administration of the correct concentration. Pre-made syringes are not always available. Can be prepared at bedside using 1 mL (0.1 mg) from a 1:10,000 epinephrine syringe. Then dilute with 9 mL of normal saline to produce a concentration of 10 mcg/mL.
Overview of Evidence
| Author, year | Design / Sample Size | Intervention & Comparison | Outcome |
|---|---|---|---|
| Panchal, 2015 | Retrospective, observational study in the ED
N = 20 |
Included hypotensive adults intubated in the ED that received at least one push-dose of PHE within 30 minutes of intubation
No comparator |
The average pre- and post-PHE SBP increased from 73 mmHg (95 percent CI 67-78) to 93 mmHg (95 percent CI 80-105), P<0.05, and DBP increased from 42 mmHg (95 percent CI 35-48) to 52 mmHg (95 percent CI 44-58). No significant effect was seen regarding heart rate. Overall, 70 percent of patients still required a CVI, of note 5 of 20 CVIs were initiated prior to PHE and 9 of 20 CVIs were initiated after PHE. |
| Schwartz, 2016 | Retrospective, observational study in the ED
N = 73 |
Included hypotensive adults that received at least one push-dose of PHE for any indication
No comparator |
Out of the 73 patients, 46.5 percent were initiated on a CVI within 30 minutes after PHE (another 14 percent were already on a CVI prior to PHE).
Subgroup analyses showed that more patients were initiated on a CVI when they received <30 mL/kg of crystalloids prior to PHE (26 of 48 patients, 54 percent) as opposed to patients who received ≥30 mL/kg of crystalloids prior to PHE (9 of 25 patients, 36 percent). The <30 mL/kg group also had a higher average of PHE doses given (2.3 versus 1.5, P=0.01). Most common adverse events seen included bradycardia (9.6 percent), reactive hypertension (8.2 percent), and ventricular tachycardia (2.7 percent). |
| Swenson, 2018 | Retrospective, observational study in the ED
N = 181 |
Included hypotensive adults that received at least one push-dose of PHE for any indication
No comparator |
The primary outcome evaluated rates of adverse events within 30 minutes of PHE administration. Of 181 patients, three patients had documented SBPs > 180 mmHg and two patients developed bradycardia.
Overall, 60 percent of patients were initiated on a CVI. |
| Cole, 2019 | Retrospective, observational study in the ED | Included hypotensive adults that received at least one push-dose of PHE (n = 110) or EPI (n = 139) for any indication | Adverse hemodynamic events occurring within 10 minutes of PHE and EPI were 27 percent and 50 percent of patients, respectively. Both groups had similar rates of human error via overdoses (2.7 percent PHE versus 2.9 percent EPI). Overall, 19 percent of all patients had some involvement of human error. Survival to hospital discharge was higher in the PHE group (64 percent) compared to the EPI group (36 percent), though this may be related to the variety of patient presentations and indications for each drug. The majority of patients in the EPI group were post-cardiac arrest, 57 percent versus 20 percent. Overall, 71 percent of patients were initiated on a CVI. |
Abbreviations: CVI, continuous vasopressor infusion; DBP, diastolic blood pressure; EPI, epinephrine; PHE, phenylephrine; SBP, systolic blood pressure
*PHE and EPI refer to push-dose administrations
 Dr. Gibbs is the chair of the department of emergency medicine at Carolinas Medical Center in Charlotte, N.C.
Dr. Gibbs is the chair of the department of emergency medicine at Carolinas Medical Center in Charlotte, N.C.
 Dr. Cason is a Clinical Pharmacy Specialist in Emergency Medicine at Carolinas Medical Center in Charlotte, N.C.
Dr. Cason is a Clinical Pharmacy Specialist in Emergency Medicine at Carolinas Medical Center in Charlotte, N.C.
References
- Cole JB, Knack SK, Karl ER, et al. Human errors and adverse hemodynamic events related to “push dose pressors” in the emergency department. J Med Toxicol. 2019;15(4):276-286.
- Kubena A, Weston S, Alvey H. Push-dose vasopressors in the emergency department: A narrative review. J Emerg Crit Care Med. 2022;6:22.
- Micromedex 2.0 (Healthcare Series), (electronic version). Truven Health Analytics, Greenwood Village, CO, USA. Available at: http://www.micromedexsolutions.com/.
- Panchal AR, Satyanarayan A, Bahadir JD, et al. Efficacy of bolus-dose phenylephrine for peri-intubation hypotension. J Emerg Med. 2015;49(4):488-494.
- Schwartz MB, Ferreira JA, Aaronson PM. The impact of push-dose phenylephrine use on subsequent preload expansion in the ED setting. Am J Emerg Med. 2016;34(12):2419-2422.
- Swenson K, Rankin S, Daconti L, et al. Safety of bolus-dose phenylephrine for hypotensive emergency department patients. Am J Emerg Med. 2018;36(10):1802-1806.





No Responses to “Phenylephrine and Epinephrine Push-Dose Vasopressors”