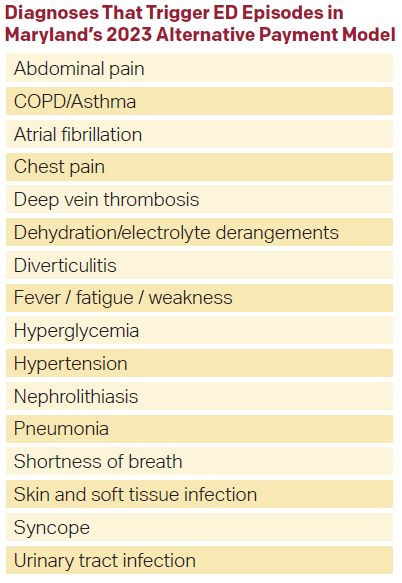
 Nevertheless, the primary way groups will be successful under this model is through implementing evidence-based protocols surrounding hospital admission because that is the primary vector for 14-day total cost of care after an ED visit. Examples include using the HEART score for chest pain admissions or atrial fibrillation discharge pathways.3 Groups also should identify high admitting emergency physicians in their practices who can be coached on using evidence-based decision rules.
Nevertheless, the primary way groups will be successful under this model is through implementing evidence-based protocols surrounding hospital admission because that is the primary vector for 14-day total cost of care after an ED visit. Examples include using the HEART score for chest pain admissions or atrial fibrillation discharge pathways.3 Groups also should identify high admitting emergency physicians in their practices who can be coached on using evidence-based decision rules.
Explore This Issue
ACEP Now: Vol 42 – No 12 – December 2023Ground Zero for Payment Models
Maryland is ground zero for payment reform because it has dedicated local mechanisms in place to administer programs through the HSCRC. Since the 1970s, a Centers for Medicare and Medicaid Services (CMS) waiver has allowed all hospital payments in Maryland to be regulated by the state’s HSCRC. This allows HSCRC to be nimble and experiment with new payment models proposed by local stakeholders. In the case of this program, it was designed by ED physicians in a partnership between state clinical leaders through the Maryland ACEP, HSCRC, MedChi (the Maryland physician society), and the Maryland Hospital Association. Additionally, the program is classified as an advanced alternative payment model (AAPM). Thus, participating physicians will also receive a 3.5 percent bonus on all Medicare claims, on top of any shared savings. Participating physicians are also not required to submit data to the Merit-based Incentive Payment System (MIPS) program through CMS, nor be subject to its rewards or penalties.
While the Maryland program is a step in the right direction for ED value-based care, it will likely serve as a temporary program, lasting only a few years. This is because all shared savings programs, like accountable care organizations (ACOs) and others, tend to have a limited shelf life. The basis of shared savings models is reducing costs of care compared to a prior baseline. This cannot occur indefinitely. Ultimately, the only durable long-term alternative payment model is global budgets for emergency physicians, similar to capitation for primary care physicians.. Emergency physician global budgets would be designed to align physician payments directly with population health goals. Maryland would be a great place to test ED physician global budgets because hospitals already receive all-payer global budgets for both inpatient and outpatient services through the state’s Global Budget Revenue (GBR) program through HSCRC. Hospital GBR has been by far the most successful alternative payment in reducing costs.4 Additionally because hospitals are already on GBR, they are already aligned with population health goals.
Pages: 1 2 3 4 | Single Page




No Responses to “Maryland Implements Value-Based Alternative Payment Model”