Technique
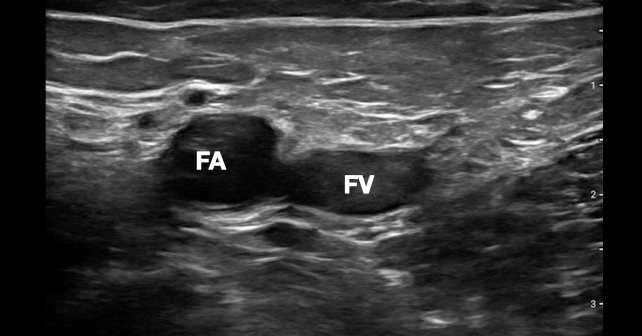
Place the linear probe at the inguinal crease and look for pulsation of the common femoral artery on B-mode. Additionally, prior to the CPR pause, press the Doppler button and move the Doppler gate over the femoral artery. When the CPR pause starts, press the Doppler button again to measure a Doppler waveform. Keeping your non-scanning hand over the Doppler button as the CPR pause approaches will minimize delay to waveform recording. Freeze the waveform image and measure the maximum amplitude of the peak systolic velocity. A value of greater than 20 cm/sec has been shown in some studies to correlate to a systolic blood pressure over 60 mmHg (see Figure 2).9
Explore This Issue
ACEP Now: Vol 42 – No 09 – September 2023Conclusion
Incorporating POCUS into the resuscitation of a patient in cardiac arrest is an important skill for the emergency physician. A protocolized algorithm and simple techniques to reduce CPR pauses allows POCUS to be integrated without the inadvertent complication of prolonging CPR pauses. Bedside imaging allows clinicians to diagnose reversible causes rapidly as well as to define endpoints for resuscitation. We use the initial steps of the CASA protocol to ensure that there are no acutely reversible causes on the first two CPR pauses, but then move to the right femoral region with a linear transducer once these steps are complete. Along with defining the presence of pulses with higher accuracy, we employ femoral artery Doppler waveform to determine the presence of a perfusable rhythm. This adjustment to our resuscitation protocol is one way to stay off the chest during compressions while also employing POCUS to help improve the care of our sickest patients.
Dr. Martin is director of resident and medical student ultrasound education at Highland Hospital/Alameda Hospital in Oakland, Calif.
Dr. Howell is an ultrasound fellow at Highland Hospital/Alameda Health System in Oakland, Calif.
Dr. Nagdev is director of emergency ultrasound at Highland Hospital/Alameda Health System in Oakland, Calif.
Dr. Desai is an ultrasound fellow at Highland Hospital/Alameda Health System in Oakland, Calif.
References
- Clattenburg EJ, Wroe PC, Gardner K, et al. Point-of-care ultrasound use in patients with cardiac arrest is associated prolonged cardiopulmonary resuscitation pauses: A prospective cohort study. Resuscitation. 2018;122:65-68.
- Huis In ’t Veld MA, Allison MG, Bostick DS, et al. Ultrasound use during cardiopulmonary resuscitation is associated with delays in chest compressions. Resuscitation. 2017;119:95-98.
- Clattenburg EJ, Wroe PC, Gardner K, et al. Implementation of the cardiac arrest sonographic assessment (CASA) protocol for patients with cardiac arrest is associated with shorter CPR pulse checks. Resuscitation. 2018;131:69-73.
- Gaspari R, Harvey J, DiCroce C, et al. Echocardiographic pre-pause imaging and identifying the acoustic window during CPR reduces CPR pause time during ACLS – A prospective cohort study. Resusc Plus. 2021;6:100094.
- Hu K, Gupta N, Teran F, et al. Variability in interpretation of cardiac standstill among physician sonographers. Ann Emerg Med. 2018;71(2):193-198.
- Kang SY, Jo IJ, Lee G, et al. Point-of-care ultrasound compression of the carotid artery for pulse determination in cardiopulmonary resuscitation. Resuscitation. 2022;179:206-213.
- Gaspari R, Weekes A, Adhikari S, et al. A retrospective study of pulseless electrical activity, bedside ultrasound identifies interventions during resuscitation associated with improved survival to hospital admission. A REASON Study. Resuscitation. 2017;120:103-107.
- Cohen AL, Li T, Becker LB, et al. Femoral artery Doppler ultrasound is more accurate than manual palpation for pulse detection in cardiac arrest. Resuscitation. 2022;173:156-165.
- Haddad G, Margius D, Cohen AL, et al. Doppler ultrasound peak systolic velocity versus end tidal carbon dioxide during pulse checks in cardiac arrest. Resuscitation. 2023;183:109695.
Pages: 1 2 3 4 | Single Page





No Responses to “How To Safely Incorporate Ultrasound Into Cardiac Arrest Resuscitation”