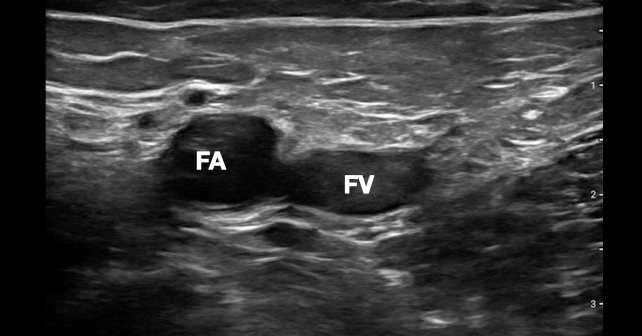
Switching to a linear probe and imaging at the common femoral artery has become our third step in our cardiac arrest ultrasound algorithm because this approach is faster and more reliable than subjectively feeling for a pulse. Ultrasound is more than twice as sensitive for the presence of a pulse than manual palpation.6 Using a linear probe to identify pulsatility of the femoral or carotid artery has been shown to be more accurate than manual palpation for pulses, and can almost always be done in less than five seconds.6 This modification removes the clinical sonographer from the chest, decreasing prolonged pauses in CPR. The simplest way to look for a pulse with ultrasound is to place a linear probe on the inguinal crease and identify the common femoral artery during ongoing compressions. The right femoral region is commonly selected because the first two steps of the CASA protocol are usually performed from the right side of the patient. The goal is to apply enough pressure to collapse the femoral vein, and look for pulsatility of the femoral artery (see Figure 2).
Explore This Issue
ACEP Now: Vol 42 – No 09 – September 2023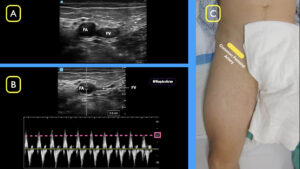
FIGURE 2: A) Compress the common femoral vein (FV) and visualize pulses in the common femoral artery (FA) B) Using spectral doppler, define a peak systolic velocity (PSV) >20 cm/sec C) Using a linear probe in the inguinal crease, locate the common femoral artery and vein. (Click to enlarge.)
In addition to using B-mode ultrasound to determine the presence or absence of a femoral pulse during a cardiac resuscitation, spectral or gated Doppler can be added at the same location to identify whether there is a perfusable rhythm. Work by Gaspari, et al., defined that some patients previously thought to have PEA are now recognized as having “pseudo-PEA,” where the heart is beating in an organized manner but a pulse cannot be manually palpated due to low cardiac output.7 This scenario raises the question of how to identify if sufficient cardiac perfusion is present that CPR is no longer needed. Recent studies show that applying gated Doppler to the femoral artery can identify patients who have achieved ROSC whether or not they have a palpable pulse.8 In practical terms, if femoral arterial pulsation is present on B-mode ultrasound during a pulse check, the next step is to use the spectral Doppler function to measure the peak systolic velocity, which may be used to define a perfusable pressure (or ROSC). This technique allows the clinician to determine the presence of a perfusable rhythm and may be even more sensitive than a rise in the end-tidal CO2, which was previously considered the first sign of ROSC.9
Pages: 1 2 3 4 | Single Page





No Responses to “How To Safely Incorporate Ultrasound Into Cardiac Arrest Resuscitation”