Explore This Issue
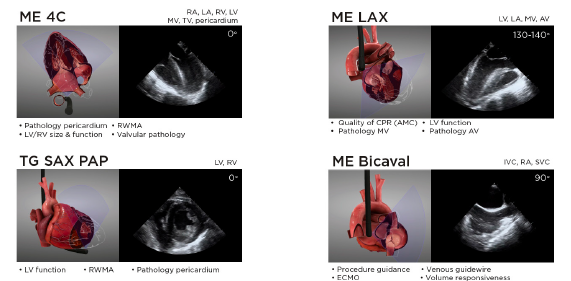
ACEP Now: Vol 39 – No 07 – July 2020Figure 6: Summary of the views and main clinical applications of the four core resuscitative TEE views. Additional views can be used on a case-by-case basis to answer questions and guide management in specific clinical scenarios. Some of these views include mid-esophageal 2C (ME 2C), mid-esophageal aortic valve and ascending aorta short and long axis (ME AV SAX, ME ascending aorta SAX/LAX), right ventricular inflow-outflow (ME RV I-O), descending thoracic aorta (DTA SAX and LAX), and deep transgastric 5 chamber (Deep TG 5C). A full protocol including additional resuscitative TEE views can be found at www.resuscitativetee.com/protocols.
The right atrium (RA) and right ventricle (RV) are relatively anterior cardiac structures. Meanwhile, the left atrium (LA) and left ventricle (LV) are posterior structures. The LA is the closest structure to the esophagus at the mid-esophageal level, so the ultrasound beam passes through this structure first. This is why mid-esophageal views have the LA located in the near field of the image and can be conceived as the scanning window to visualize the heart in TEE. The heart lies anterior and slightly left in relation to the esophagus, with the LA “leaning” against the esophagus. The right heart is situated anteriorly within the mediastinum and is the farthest structure from the esophagus, which is why, unlike in TTE, in TEE the RV is seen in the far field of the image.
Imaging Planes and Resuscitative TEE Views
Four core TEE views are most commonly used in resuscitative settings and provide the highest yield of information. These include mid-esophageal 4 chamber (ME 4C), mid-esophageal long axis (ME LAX), transgastric short axis at the level of papillary muscles (TG SAX PAP), and mid-esophageal bicaval (ME bicaval).
Developing the cognitive and motor skills needed to acquire and interpret these views proficiently, like any other imaging modality, takes practice. In our experience, simulation training is essential in both skill acquisition and maintenance of competency. Therefore, we recommend that clinicians who would like to incorporate TEE into their clinical care find a resuscitative TEE hands-on course to provide them with structured training, then supplement that training with mentored training in live patients (see Figure 6).
Conclusion
Emergency medicine has rapidly developed from its early days into a dynamic field in which experts push boundaries in optimal clinical care. Resuscitative TEE is yet another attempt to both define our growing specialty while offering the best care for our critically ill patients. Acute care physicians (including emergency medicine) will continue to define indications of TEE and to expand the field, integrating this novel technology into our scope of practice.
Today, it has become standard for many ED clinicians to perform bedside transthoracic ultrasound in the evaluation of a hypotensive or dyspneic patient. In the near future, TEE will become another invaluable tool during the resuscitation in the emergency department.
As William Gibson once said, “The future is here. It’s just not evenly distributed yet.”





No Responses to “How to Perform Resuscitative Transesophageal Echocardiography in the Emergency Department”