Bedside transthoracic echocardiography (TTE) has become an invaluable tool in emergency and critical care medicine. Bedside assessment of the presence or absence of a pericardial effusion, gross ejection fraction, size of the right ventricle, and cardiac activity during cardiopulmonary resuscitations has become standard in residency training and general practice.1
Explore This Issue
ACEP Now: Vol 39 – No 07 – July 2020In the past few years, a growing group of emergency department sonographers has
pioneered work in how transesophageal echocardiography (TEE) performed at the bedside may provide similar utility. Like the previous generation of clinicians who were able to teach legions of ED sonographers to perform various exams at the bedside, these sonographers have helped the availability of TEE at the bedside start to become a reality.
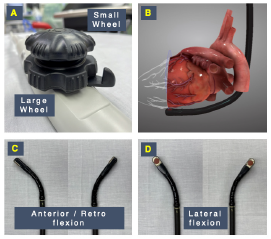
Figure 2: Mechanical controls of a TEE probe. (A) A large wheel controls anteflexion, as required to obtain a transgastric short axis view (B) and retroflexion (C). A small wheel performs lateral flexion (D).
TEE offers a few clear advantages over the classic TTE performed in most emergency departments today. First, because the probe visualizes the heart through the esophagus, the windows are excellent and easy to obtain (the lungs, ribs, and habitus do not interfere). Second, TEE allows the sonographer to be off the chest during active CPR, facilitating visualization of the heart continuously to guide management while not interrupting compressions. TTE can be used for assessing fluid responsiveness in mechanically ventilated patients, the guidance of pacemaker placement, and the guidance of extracorporeal membrane oxygenation (ECMO) cannulation during initiation of extracorporeal circulation (ECPR).
Given its reliability in providing high-quality images regardless of patient-related or external factors that often limit TTE, TEE represents a powerful tool for the delivery of critical care.2–4
Once a modality used only for comprehensive examinations, over the last two decades TEE has expanded from its traditional diagnostic indications (ie, cardiac surgery, suspected endocarditis, or cardioversion in atrial fibrillation) to assist the evaluation and management of patients with acute hemodynamic decompensation, shock, and cardiac arrest in operative and nonoperative environments.
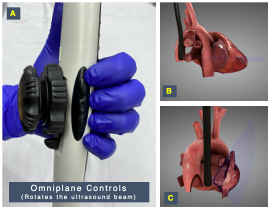
Figure 3: (A) Lateral buttons allow for digital rotation of the ultrasound beam (omniplane) generated in the probe head. (B) Rotation between 0° and 180° using these buttons allows the probe to develop views in multiple planes such as coronal or transverse (note the purple omniplane axis). (C) The four-chamber view or sagittal plane in a bicaval view is shown for comparison.
3-D graphics reproduced with permission by HeartWorks Intelligent Ultrasound
The use of TEE in the emergency department and critical care settings, often defined as “focused” or “resuscitative” to describe its goal-directed nature and differentiate the scope and objectives of application from comprehensive or consultative TEE, has been shown to be feasible, safe, and clinically impactful in the emergency and intensive care settings, and its use has been supported by society guidelines.1–4
In this article, we aim to provide a practical overview on the use of resuscitative TEE for emergency physicians.





No Responses to “How to Perform Resuscitative Transesophageal Echocardiography in the Emergency Department”