- Position the patient supine, in the seated position with hips in slight flexion (to prevent patellar tendon contraction).
- Use one hand to maintain support near the ankle.
- While applying medial pressure to the lateral patella, passively extend the knee slowly.
- The physician should note a click as the patella slides back into the femoral groove.
- Confirm with post-reduction anteroposterior and lateral radiographic views.
Post-reduction, the patient should be placed in a knee immobilizer to take away the flexion and extension mechanism of the knee. They should be non-weight-bearing (using crutches). All physical activity and sporting events are prohibited until cleared by orthopedics at follow-up. Most uncomplicated first-time dislocations can be managed nonoperatively with physical therapy and a slow return to play. Recurrent or complicated dislocations involving osteochondral injuries or instability can require elective surgical intervention.
Explore This Issue
ACEP Now: Vol 40 – No 03 – March 2021Reduction of a knee dislocation should be attempted with procedural sedation in consultation with orthopedic surgery if possible. The first attempt should involve simple longitudinal traction. If this is unsuccessful, the next step is to attempt to reverse the direction of the deforming force:18
- In an anterior knee dislocation, push the tibia posterior while simultaneously lifting the distal femur.
- In a posterior knee dislocation, lift the tibia anteriorly while simultaneously placing pressure over the femur.
- If these reduction techniques are unsuccessful, operative management under anesthesia is indicated.
Post-reduction, radiographs should be obtained immediately to confirm a successful reduction, and the patient should be placed in a splint at 20 degrees of flexion. The splint should be constructed such that posterior subluxation of the tibia is prevented while also minimizing vascular traction. The splint should be windowed to allow for repeat vascular exams of the foot.18
Summary

Figure 7: X-ray showing knee dislocation in a patient with a total knee arthroplasty. Credit: John Kiel
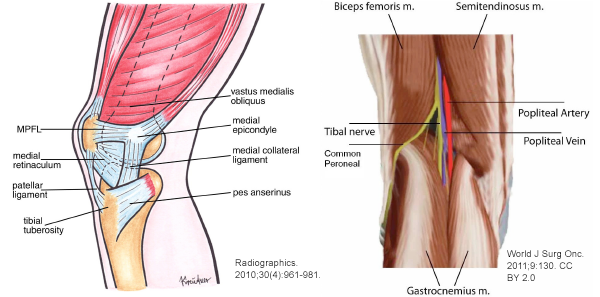
Understanding the differences between patellar and knee dislocations is imperative for recognizing and preventing potentially catastrophic complications (see Table 1). Patellar dislocation is an injury that occurs most commonly in young and active individuals. The majority of patellar dislocations will reduce spontaneously prior to ED arrival. Knee dislocation is an injury that can present similarly and should be in the considered differential diagnosis based on mechanism, examination, and clinical gestalt. This injury usually involves high-energy mechanisms. About 50 percent of cases will reduce spontaneously prior to ED arrival, thus a thorough knee examination is critical; careful neurovascular evaluation of the lower-extremity status must be performed. If there is evidence of vascular injury, the patient requires emergent revascularization with vascular surgery, as ischemia time is correlated with risk of amputation.
In the emergency department, reduction of patellar dislocations is generally straightforward. Post-reduction radiographs should be obtained and the patient placed in a knee immobilizer. This injury does not require orthopedic consultation in the emergency department; however, patients should follow up with orthopedic surgery as an outpatient within one to two weeks. Return to play should be individualized toward the athlete and the activity, but main treatment goals prior to return to play are lower-limb stabilization, strengthening of the quadriceps and gluteus medius muscles, and avoidance of specific high-risk movements. Knee dislocation reduction in the emergency department typically requires simple longitudinal traction with pre- and post-reduction radiographs and neurovascular exam. Post-reduction testing typically involves an ABI and often a CT angiogram. All patients with knee dislocations require orthopedic consultation in the emergency department and often vascular/trauma services as well. The affected extremity should be splinted at 20 degrees, and the patient should be admitted for 24-hour observation with serial vascular exams. In follow-up, the patient may require staged reconstruction or repair of the injured ligaments and other soft tissue structures.
Table 1: Comparison of Patellar Dislocation and Knee Dislocation
| Patellar Dislocation | Knee Dislocation | |
|---|---|---|
| Mechanism | Noncontact twisting injury (flexion with external rotation) or direct blow (often sports-related) Anatomical risk factors |
High-energy mechanisms (eg, trauma, motor vehicle accidents, sports) Morbid obesity |
| Physical Exam | Majority spontaneously reduce Painful laterally displaced patella Neurovascularly intact |
50% spontaneously reduce Painful anterior, posterior, or lateral disarticulation of femur and tibia Structural examination of knee Assess neurovascular status |
| Complications | Recurrent dislocations Patellofemoral pain or arthritis Osteochondral defect |
Arthrofibrosis (most common) Popliteal artery injury Amputation Peroneal nerve injury Chronic pain or persistent knee instability |
| Imaging | Pre-reduction radiographs: if fracture suspected Post-reduction radiographs: always |
Pre-reduction radiographs to assess for concomitant fracture Post-reduction radiographs Well perfused with absent/asymmetric pulse: CT angiography Well perfused with normal pulse: Ankle Brachial Index (ABI) |
| Reduction | Pre-reduction analgesia or sedation not typically required Apply medial pressure to the lateral patella, passively extend the knee slowly |
Requires procedural sedation Attempt simple longitudinal traction first If fails, reverse direction of the dislocation If both fail, move to operating room for reduction under anesthesia Post-reduction neurovascular assessment |
| Management | If subluxated, reduce and obtain post-reduction radiograph If reduced prior to emergency department, confirm extensor mechanism intact (have patient extend leg or evaluate via ultrasound) Place in knee immobilizer |
Reduce under procedural sedation Post-reduction ABI or CT angiography based on pulse status If evidence of vascular injury or hard signs of ischemia, move to operating room and obtain vascular surgery consult immediately (do not delay for imaging) If no emergent vascular injury, place in splint at 20 degrees flexion, admit for 24-hour observation with serial exams |
| Consultation | Does not require orthopedic consultation in the emergency department | Requires orthopedic consult and often vascular/trauma services |
| Disposition | Discharge home and counsel on complications, return-to-play goals Outpatient orthopedic follow-up in 1–2 weeks |
Admit for serial examinations based on consult discretion |
Case Resolution
The patient’s deformity was consistent with a laterally dislocated patella. The limb was well perfused, with no neurovascular insult. The injury was successfully reduced in the emergency department after administration of IV fentanyl. A knee immobilizer and crutches were provided. Outpatient follow-up with orthopedic surgery and physical therapy was arranged.





No Responses to “How To Identify and Treat Patellar Dislocation Versus Knee Dislocation”