Pathophysiology
In 93 percent of patellar dislocations, the mechanism involved is a flexion and valgus movement of the knee without direct contact. Noncontact mechanisms often involve a twisting injury with the foot externally rotated and the knee extended, while traumatic causes typically involve a direct blow to the knee. There are also a number of predisposing factors that increase risk of patella dislocation in individuals. One such risk factor is trochlear dysplasia, where the trochlear groove is flat or convex as a result of gradual filling of the trochlear floor.10 Another predisposing factor to patellar dislocation is a high-riding patella (patella alta). When the patellar tendon is too long, the patella bone sits superior to the trochlear fossa.11
Explore This Issue
ACEP Now: Vol 40 – No 03 – March 2021Knee dislocation usually requires higher-energy mechanisms. However, a low-energy dislocation mechanism has been documented in patients with morbid obesity. Popliteal artery injury is reported in 18 to 64 percent of knee dislocations, with 12 percent of these cases requiring amputation. The amputation rate in patients with popliteal ischemia for greater than eight hours is 86 percent, thus early intervention is crucial if this diagnosis is suspected.12,13 Peroneal nerve injury is another potential complication. Nerve injury is seen in 25 to 33 percent of knee dislocations and is more commonly seen in sports-related injuries.14 It is worth noting that knee dislocations, with or without spontaneous reduction, may present with other significant traumatic and life-threatening pathology.
Clinical Features and Physical Exam
In the majority of patellar dislocation cases, the patient will have subluxed or dislocated with spontaneous reduction prior to arrival to the emergency department. Thus, it is critical to clarify the mechanism of injury and symptoms prior to arrival. Only 20 percent of patellar dislocations require reduction in the emergency department.10 In patients whose dislocations do not resolve spontaneously, most will be evident with visible lateral deviation of the patella (see Figure 3).
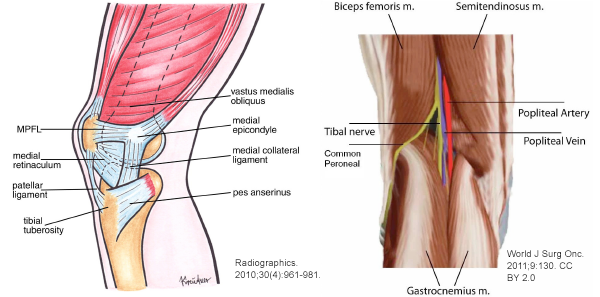
Most patients present in obvious discomfort, often with the knee held in slight flexion. A joint effusion may be present. Distally, the patient should be neurovascularly intact as the popliteal bundle is posterior to the femorotibial joint and unaffected by this injury. It is important to confirm the quadriceps and patellar tendons are intact by assessing active and passive leg raise against gravity and/or with point-of-care ultrasound. Clinical exam findings that suggest a subluxation or spontaneous dislocation reduction prior to arrival include tenderness of the medial femoral condyle (attachment site of the MPFL) or lateral femoral condyle (where the patella likely collided with the lateral femur during the event).
Knee dislocations can be clinically obvious with a significant mechanism and gross deformity. However, many knee dislocations spontaneously reduce, and about 50 percent appear normal with no obvious deformity on initial presentation.15 Given that this injury often involves high-energy mechanisms, it is important to evaluate for other injuries. If a patient presents with acute trauma to the knee, it is important to evaluate for more subtle signs such as joint effusion, swelling, and ecchymosis. In an acute knee dislocation, there may be a dimple sign or buttonholing of the medial femoral condyle through the capsule. Structural examination of the major knee ligaments should be performed, including anterior and posterior drawer test and varus and valgus stress test, at minimum. All lower-extremity pulses should be assessed and documented when there is concern for knee dislocation due to possible injury to the popliteal artery, which is the most feared complication. Early recognition and intervention for this vascular injury is associated with decreased likelihood of complications. Vascular injury resulting from knee dislocation can present as a pulseless lower extremity. Conversely, the presence of peripheral pulses in the lower extremity alone does not exclude a vascular injury, so serial vascular exams must be performed.15 Other signs of vascular injury can include pallor, cold limb, ecchymosis, and paresthesia. If vascular injury is suspected or confirmed, vascular surgery should be consulted immediately. Even if this injury spontaneously reduces before presentation to the emergency department, the risk of vascular injury remains. To assess for nerve injury, a motor and sensory exam should be performed and documented. With peroneal nerve injury, weakness of ankle dorsiflexion, or “foot drop,” is most common. There may also be numbness or paresthesia along the lateral leg and dorsum of the foot.16





No Responses to “How To Identify and Treat Patellar Dislocation Versus Knee Dislocation”