Explore This Issue
ACEP Now: Vol 40 – No 03 – March 2021The Case
A 15-year-old boy presents to the emergency department with acute left knee pain. While playing football, he was tackled with his left knee planted and experienced a sudden pain. He was unable to ambulate after the injury. On exam, he is in severe discomfort and tachycardic and has an obvious deformity of his left knee.
Discussion
Patellar dislocations and knee dislocations, though often mistakenly used interchangeably, are different clinical entities with distinct mechanisms and presentations.
Patellar dislocation occurs when there is disarticulation of the patella bone from the patellofemoral joint. It usually occurs from low-to-moderate trauma sustained during sports or other physical activity. Risk factors for patellar dislocation include structural variants of the patella or femoral trochlea, ligamentous laxity, trauma, and connective tissue disorders. Patellar dislocations represent 3 percent of knee injuries, with a high recurrence rate ranging from 15 to 44 percent for first-time dislocations and 50 percent with a previous history of two or more dislocations.1,2 The risk of patellar dislocation injury is highest in females ages 10 to 17 years old, with an incidence of 29 per 100,000.2 The mechanism in the vast majority of patellar dislocations is noncontact involving knee flexion, a valgus force with external rotation. Patients with patellar instability can struggle to return to sports and develop functional limitations, arthritis, and chronic pain.1,2
Knee dislocation is a dislocation of the tibia with respect to the femur and is seen in high-energy traumas including motor vehicle accidents, falls from heights, industrial injuries, and sports injuries, as well as spontaneously in the morbidly obese during ambulation.3 Knee dislocations involve disruption of major knee-stabilizing ligaments (medial collateral ligament, posterior cruciate ligament, anterior cruciate ligament, lateral collateral ligament, and posterolateral corner). Meniscal tears are seen in about 50 percent of cases, and fractures are seen in about one-third of cases.4,5 Knee dislocations are substantially less common than patellar dislocations, with slightly higher incidence in males and a mean patient age of 35.6 Anterior knee dislocations are more common and account for 40 percent of all knee dislocations.7 We will discuss key differences between these injuries, their complications, and respective ED management.
Anatomy and Biomechanics

Figure 3: Visible lateral deviation of the patella. Credit: Radiographics. 2010;30(4):961-981.
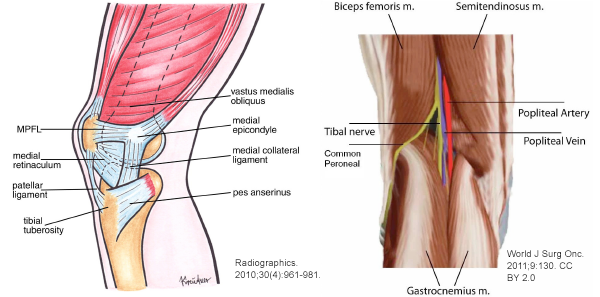
The patella acts as a lever arm connecting the quadriceps muscles via the quadriceps tendon to the tibia via the patellar tendon. Collectively, this unit is responsible for knee extension and is often referred to as the “extensor mechanism.” The patellofemoral joint refers to the articulation of the patella within the trochlear groove of the femur. Patellar instability can be derived from any anatomical change in the patellofemoral joint. The vastus medialis obliquus muscle and medial patellofemoral ligament (MPFL) are responsible for much of the medial stability of the patellofemoral joint by counteracting the natural lateral glide of the patella (see Figure 1).8
Knee dislocations are associated with more dangerous complications because injuries involving this structural complex can be associated with vascular and/or nerve injury. The primary stabilizer ligaments of the posterolateral corner are the popliteus tendon, fibular collateral ligament, and popliteofibular ligament. Both the long and short head of the biceps femoris muscle act as secondary stabilizers here.9 Running through the popliteal fossa at the level of the tibiofemoral junction are the popliteal artery and vein, tibial nerve, and common fibular (peroneal) nerve (see Figure 2).





No Responses to “How To Identify and Treat Patellar Dislocation Versus Knee Dislocation”