Trap #2: Chest pain plus anxiety and neurological complaints. What if the anxiety is not the cause of the neuro symptoms?
1. A 55-year-old female with a history of GERD has rapid onset of epigastric pain, right hand numbness, blurry vision, and decreased sense of taste. ECG, CXR, and troponin are all normal. She is diagnosed with anxiety and given alprazolam, and dies eight hours later of aortic dissection.
Explore This Issue
ACEP Now: Vol 42 – No 06 – June 20232. A 38-year-old male feels a “pop” in his chest while lifting weights, followed a minute later by severe pain radiating into both legs. He arrives in the ED stating, “I can’t move my legs.” A consulting surgeon notes that he “is able to move his legs” and suspects malingering. He is given morphine and sent for a CT scan of the lumbar spine which reveals “multiple lumbar disc herniations.” While awaiting admission for “intractable back pain,” he dies of pericardial tamponade. A later review of the CT scan shows a visible abdominal aortic dissection flap that was missed.
Takeaway: Chest pain with neuro symptoms and anxiety can be the yellow brick road to disaster. Thoracic pain and any neurological complaint must include aortic dissection in the differential.
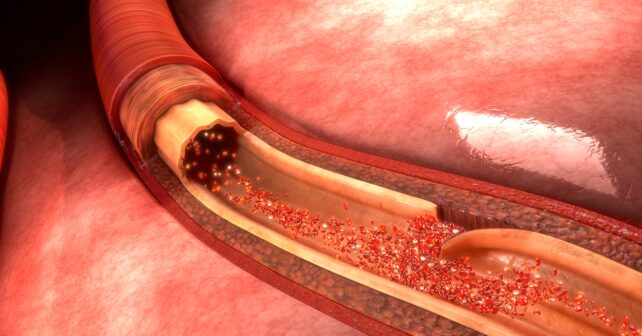
Any artery can be affected (e.g., a dissection can mimic lumbar disc herniation when it extends into the anterior spinal artery causing sudden paraplegia), which can wax and wane. Adding to the temptation to attribute the patient’s symptoms to anxiety, micro-emboli from a dissection’s turbulent flow can cause scattered, non-anatomic, sensorimotor symptoms, (e.g., loss of taste or tongue and hand numbness). And only a psychiatrist is allowed to use the word “malingering” in a medical record.
Trap #3: You’re too young to have an aortic dissection.
A 20-year-old male pushes a car up a hill when he notes sudden chest pain. An ECG and CXR are negative. He is given morphine for “costochondritis” and is discharged. He sees his primary doctor the next day, who schedules a stress test. The next day he collapses and dies. An autopsy shows a typical aortic dissection with tamponade and a bicuspid aortic valve.
Takeaway: Young people can have an aortic dissection, especially those with Marfan syndrome.
Trap #4: It’s been going on for days so you’re probably fine.
A 64-year-old smoker with hypertension develops chest pain and “pressure” in his neck. An ECG, CXR, and two troponins are normal. Symptoms improve with nitroglycerin and 1 mg of intravenous morphine. He is discharged and returns 4 days later with worse chest pain aggravated by breathing or moving. ECG, CXR, and troponins are again normal. He is again discharged and returns in another four days with chest pressure radiating to his right back and neck, left arm weakness, and shortness of breath. A third ECG and troponin are normal, but the CXR now shows the heart size to be at the “upper limits of normal.” A cervical CT is ordered and shows only degenerative joint disease. He is sent home a third time and dies of an aortic dissection four days later. The most recent CXR is reread and reported as showing a widened mediastinum.
Pages: 1 2 3 | Single Page





No Responses to “How To Avoid Missing an Aortic Dissection”