A 50-year-old female develops chest pain radiating to the neck and left arm. ECG, CXR, and troponin are negative. She is given morphine for pain. Four hours later she develops back pain and bilateral leg paresthesias. CT angiography shows aortic dissection which is treated surgically, but she is left with paraplegia.
Explore This Issue
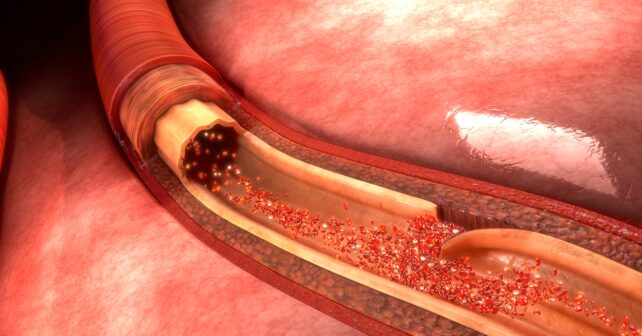
ACEP Now: Vol 42 – No 06 – June 2023Notoriously elusive, with a high misdiagnosis rate, thoracic aortic dissection (AD) can mimic many conditions, including acute coronary syndrome (ACS, the most common), gastroesophageal reflux disease (GERD), stroke, and spinal-cord compression.1 Opioids or anxiolytics are often given to patients whose diagnosis of AD is missed or delayed. The fact is that no benign thoracic disease such as non-ischemic ACS or GERD should require morphine or benzodiazepines.
The varied clinical presentations described below illustrate some of the many faces of AD.
Trap #1: Walks like a duck, quacks like a duck, but it’s not a duck. Then what?
1. A 42-year-old male develops sudden anterior chest pain radiating to his jaw while eating. He denies back pain. A medical student reports a murmur, not documented by either the emergency physician or the cardiologist. Troponins #1 and #2 are borderline and ECG is non-specific. The patient is admitted for ACS to a cardiologist who says he will see the patient in the morning. An echocardiogram the following morning shows 4+ aortic regurgitation and aortic dissection. The murmur is readily auscultated. The patient is treated surgically and survives.
2. A 35-year-old male develops sudden chest pain during an argument with his girlfriend over the phone. EMS is called and finds his blood pressure 175/100. He is given aspirin 162 mg and two doses of nitroglycerin, and his pain improves. On arrival his blood pressure is 126/90. In the ED, his troponin, ECG, and chest X-ray (CXR) are normal. He is given alprazolam for persistent symptoms and discharged. An aortic dissection is discovered when he bounces back to the ED. He survives.
Takeaway: AD does not have a classic presentation. In fact, 7 percent of ADs have none of the triad of acute tearing chest or back pain, mediastinal widening, or pulse or blood pressure differential. ACS is the most common misdiagnosis and often leads to inappropriate anticoagulation.1,2 Too often AD is missed due to anchoring or confirmation bias, where one assumes that the evidence supports one’s initial opinion. When the initial chest pain workup is complete, but the numbers don’t add up, broaden your differential. Listen to your gut. Morphine and benzos are rarely needed for stable ACS. Avoid looking for evidence to support your initial impression and instead start looking for evidence to prove yourself wrong.
Pages: 1 2 3 | Single Page





No Responses to “How To Avoid Missing an Aortic Dissection”