Consider how mobile ECMO retrieval teams may be used to maximize ICU care at referral facilities. Once patients have failed conventional hypoxemia therapies, they will be too unstable for transport without ECMO. Coordinate with neighboring ECMO centers to exchange experience and knowledge, and potentially develop care guidelines for this patient population.
Explore This Issue
ACEP Now: Vol 39 – No 04 – April 2020Intubation and Respiratory Support
Personnel from critical care, respiratory therapy, and anesthesiology should convene to develop approaches to support for suspected or confirmed COVID-19 patients with respiratory failure. Controversy exists about the use of noninvasive positive pressure ventilation and high-flow nasal cannula, which may disperse secretions and therefore virus.
We have opted to perform early tracheal intubation for these patients with placement on mechanical ventilation with a viral filter. Intubation should occur ideally in negative pressure rooms using airborne precautions.
- The intubating clinician should use a PAPR with shroud and follow donning/doffing procedures.
- Additional staff should be minimized (ideally, one nurse and one respiratory therapist).
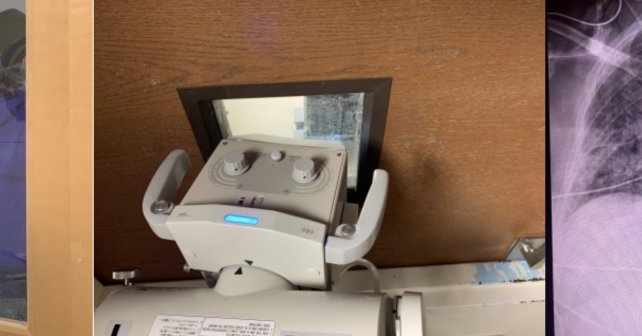
- We favor the use of video laryngoscopy to increase the distance between the intubating clinician and patient’s aerodigestive tract along with the rapid sequence intubation technique to minimize coughing or dispersion of secretions during bag-mask ventilation.
- Viral filters can be placed in-line with bag-valve masks.
- If sidestreamwaveform capnography devices are used, make sure a viral filter is placed in-line proximal to the end-tidal CO2 adapter (ie, directly on the end of the endotracheal tube, mask, or laryngeal mask airway). Otherwise, contaminated secretions may theoretically leak into the end-tidal CO2 tubing and perhaps back to the monitoring module.
Code Blue/Clinical Emergency Response
A dedicated plan for response to clinical emergencies should be created for patients with suspected or confirmed COVID-19. The plan should include limiting responding personnel, ensuring isolation precautions are maintained, and limiting aerosolizing procedure.
Consider appointing a dedicated isolation “captain” to ensure only essential staff enter the room, appropriate PPE are used, and equipment is decontaminated appropriately. The plan should include early discussions about “do not resuscitate” status with next of kin for critically ill infected patients.
The authors are in the department of emergency medicine at the University of Washington, Harborview Medical Center in Seattle.





No Responses to “Get Your Emergency Department Ready for COVID-19”