Training
Explore This Issue
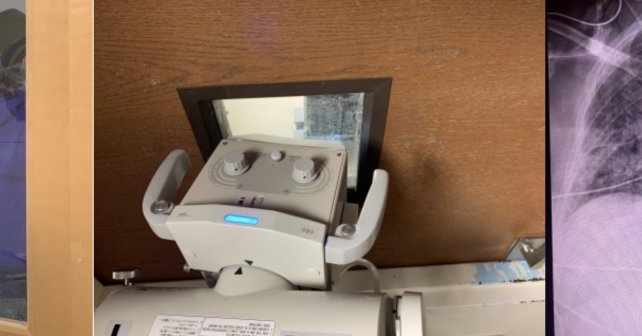
ACEP Now: Vol 39 – No 04 – April 2020Arrange in-person donning/doffing training by “supertrainers” for all ED staff. Once an airway plan has been established, use simulation training to get staff comfortable with new procedures and protocols (eg, intubating using the glidescope while in a PAPR with a shroud, as shown in Figure 2).
Tracking Systems
Review the current system or create a new one for tracking exposures and symptoms when a COVID-19 exposure happens for staff or when staff members are sick. For example, when will they return to work, and how will they get their test results?
Intubation and Airway Algorithms
Review plans for limiting staff exposure to aerosolization of COVID-19. Consider not using high-flow nasal cannula or noninvasive positive pressure ventilation in the emergency department unless adequate airborne isolation can be guaranteed and limiting use of nebulized medication. Intubation should occur only by those trained in how to intubate while in a PAPR with shroud. Follow a COVID-19-specific protocol for intubation developed by your hospital’s airway leads.
Consider PPE use, use of video laryngoscopy, premade medical airway bags, reentry and intubation checklists, and rapid sequence intubation to decrease aerosolization of particles with bag-valve masks.
Review methods for addressing severe hypoxemia and acute respiratory distress syndrome (ARDS) with ventilation, medication, and other maneuvers with all staff (eg, titration positive end-expiratory pressure, neuromuscular blockade, recruitment maneuvers, and proning).
Bundle Care
Plan ahead for blood draws, ECGs, and medication administration to minimize trips into and out of the patient’s room. Build kits with preassembled supplies to be used in isolation areas. Establish protocols for testing patients in conjunction with your lab’s ability to run these tests.
Create scripts for 911 call centers to ask about COVID-19 risk factors before sending EMS to a scene. Develop scripts for your transfer center to use screening questions regarding symptoms and COVID-19 status with the goal of identifying potential COVID-19 patients prior to ED arrival. Have EMS call ahead to alert emergency department to high-risk COVID-19 patients from the field. Draft outward-facing documents with clear instructions for the community to call their doctor prior to coming to the emergency department to reduce overcrowding.
Interfacility Triage
If your center is a receiving center for stroke or other transfers, ensure that there are COVID-19 screening questions being asked by all accepting physicians and services.
Extracorporeal Membrane Oxygenation (ECMO)
Consider risks and benefits of citywide and regional referral of patients to ECMO centers. Risks of transport may include disease spread, risk to transport personnel, and overwhelming ECMO centers’ general ICU resources. Develop strict criteria for ECMO initiation only to those with the highest chance of survival given the high number of potential ECMO candidates and limited capacity. If patients require transfer from low-resource hospitals, consider triaging potential ECMO candidate patients (young, otherwise healthy, single organ failure) to large urban ECMO centers. This may decrease the frequency of patient transports for eventual ECMO referral.





No Responses to “Get Your Emergency Department Ready for COVID-19”