Editors’ Note: This article was accepted on March 13, 2020, and was accurate at that time. Because information about SARS-CoV-2 and COVID-19 is evolving rapidly, please verify these recommendations and information.
Explore This Issue
ACEP Now: Vol 39 – No 04 – April 2020Over the course of these past several weeks, our area hospitals have been crafting a set of rapidly evolving protocols to combat the spread of SARS-CoV-2, the novel coronavirus that causes COVID-19, and develop best practices to care for our COVID-19 patients.
Since the outbreak began, our colleagues locally and nationally have been reaching out to us for assistance as they start to see cases. We hope that by sharing our work, we can assist your teams and facilities to prepare and move more quickly.
Though protocols are frequently being revised as we learn more, there are several ways to ready your emergency departments for these patients. These include creative approaches to staff training, improvements in the physical space for isolation capacity, equipment to procure/inventory, and systems for providing patient care to minimize staff exposure.
We hope you can benefit from these recommendations while you have the time to prepare yourselves and your departments. The most important and time-critical component of COVID-19 response protocol is communication.
Consider Activating Your Incident Command System
Your incident command system should include communication early and often between emergency departments, hospitalist services, ICUs, local and state departments of health (DOHs), emergency medicine services (EMS), leads, and outreach leads to vulnerable populations (eg, local skilled nursing facilities [SNFs], jails, homeless shelters). In our experience, SNFs have been particularly vulnerable and have been the source of most patients and fatalities.
Developing communication links with local SNFs for the purpose of creating a transportation and hospital disposition plan prevents proximately located hospitals from being overwhelmed by a single SNF experiencing an outbreak.
The following cheat sheet is in the staff/stuff/space/systems format of simple ideas to consider for preparing.
Staff
Initiation of Staff Preparations
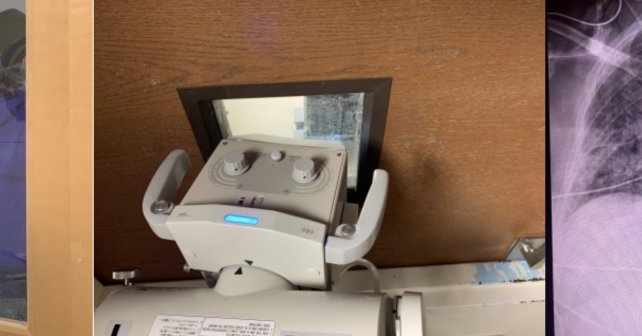
Fit testing for airborne precautions should be up-to-date within the last month for all staff, including radiology, maintenance, housekeeping, and other ancillary staff. Every physician and nurse should attest to watching the proper donning/doffing technique recommended by the Centers for Disease Control and Prevention (CDC) in the links in the “Resources” sidebar, and in-person training should be considered.
Staff should update their own home personal safety plans, including creating backup child care plans and stocking household supplies so that when work gets busy, their home plans and supplies are ready and they can concentrate on work.





No Responses to “Get Your Emergency Department Ready for COVID-19”