As a 47-year-old woman in medicine, I am accustomed to the balancing act we perform regarding our families, careers, and our well-being. In March 2024, I was planning my next six months, as we typically do in emergency medicine. I was accepted into a part-time master’s degree program at Georgetown University. I was looking forward to my mother’s birthday cruise to Alaska, and was gearing up for my 14th medical mission trip, this time to Malawi.
Explore This Issue
ACEP Now: July 2025I had my mammogram on a Friday afternoon and by Monday morning, I was called with the report of a spiculated mass in my right breast. That word just stuck in my head—spiculated.
I quickly scheduled an ultrasound, which also revealed the mass. The radiologist awkwardly delivered the news to me, without making eye contact. The ultrasound technician shooed her out and explained that I needed an ultrasound-guided biopsy. I had to wait two weeks before getting the definitive diagnosis, and during this time, I did not tell anyone what was happening. I researched breast cancer programs in the area and looked up everything I could about breast cancer diagnosis, treatment, and prognosis while waiting for the biopsy.
I also marveled at how burdensome it was for people with less flexible schedules to make these appointments. After the biopsy confirmed ductal carcinoma in situ, I was determined to get through this and back to my life.
Starting Treatment
I finally told my husband, who went with me to my breast surgeon appointment. He is not in the medical field but was there for support and a second set of ears. The plan was to get a lumpectomy with lymph node biopsy at the end of May 2024, after my mother’s birthday cruise. I told my boss, who was amazing in getting my schedule cleared for surgery and recovery. I had physical therapy, medical oncology, lymphedema clinic, and radiation oncology appointments to schedule. The day after my surgery, I finally told my immediate family and close friends. I was overwhelmed by the number of people who confessed to skipping their routine mammograms because they didn’t have the time.
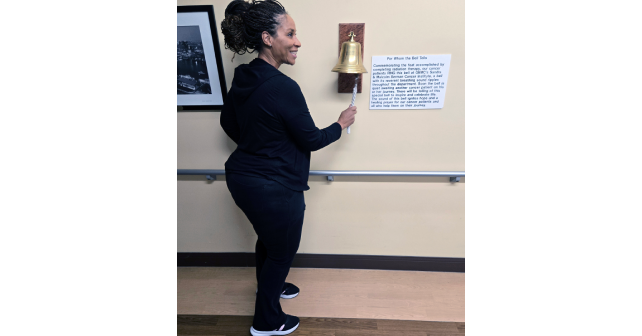
I was prepared to cancel my mission trip to Malawi, but with the blessing of my radiation oncologist, I was able to reschedule my radiation therapy. Unfortunately, my treatments were scheduled to coincide with my first classes at Georgetown. The radiation was scheduled at 7:45 a.m., every weekday for three and a half weeks. I would wake up, drive to my radiation treatment, and on class days, immediately drive one and a half hours to campus. On workdays, I would go home to nap and then work my shift. It was exhausting. In mid-September, I completed my radiation treatments and rang the bell.
Pages: 1 2 | Single Page





No Responses to “Doctors: Sharing Our Personal Health Stories Can Save a Life”