Annually, more than 300,000 adults older than age 65 are hospitalized for hip fractures, which frequently result from ground-level falls.1 Emergency medical professionals are tasked with providing care and analgesia for patients with femoral neck fractures. Monotherapy with intravenous opioids can often lead to undesired complications (eg, delirium, diminished respiratory drive, and nausea).2–4 The ultrasound-guided femoral nerve block (USGFNB) and ultrasound-guided fascia iliaca compartment block (USGFICB) offer improved pain control as well as reduced side effects in comparison with monotherapy with intravenous opioids.4,5
Explore This Issue
ACEP Now: Vol 37 – No 01 – January 2018Even though USGFNB has been described extensively in the emergency medicine literature, its use has not become commonplace. The perceived technical difficulty of the USGFNB may contribute to its current underutilization in acute traumatic femoral neck fractures.6,7 However, the USGFICB may be a potentially easier technique for the novice sonographer. Evidence supporting this theory includes the technique’s proven efficacy in the hands of a variety of clinicians, including resident physicians, nurses, and paramedics.8–10
Anatomy
Sensory innervation of the femoral neck is primarily provided by articular branches of the femoral nerve with minor contributions from the obturator nerve and the superior and inferior gluteal nerves. The femoral nerve (L2–L4) and the obturator nerve (L2–L4) both transverse a compartment that spans the lower abdomen and anterior thigh and is confined anteriorly by the fascia iliaca (ie, fascia iliaca compartment). While both the femoral and obturator nerves course through the same compartment, deposition of large volumes of local anesthesia under the fascia iliaca (as with USGFICB) seldom successfully blocks the obturator nerve.11 That said, available evidence also suggests that the obturator nerve minimally contributes to distal sensory innervation.12
To perform a USGFICB, two approaches exist. Both have the goal of injecting local anesthetic into the compartment lateral to the femoral nerve, which lies lateral and adjacent to the vascular bundle (see Figure 1). The two approaches are the infrainguinal (see Figure 2A) and the suprainguinal (see Figure 2B).
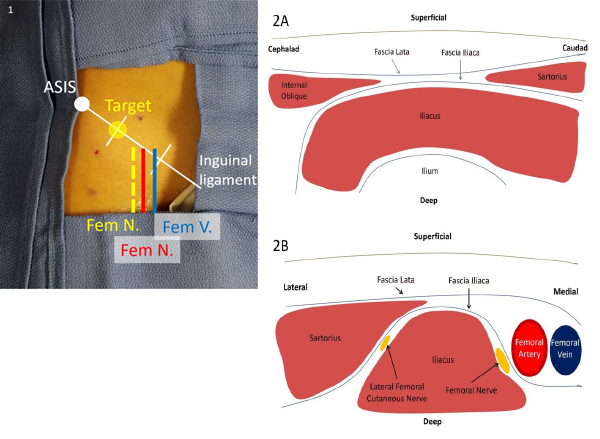
Figure 1. The inguinal ligament may be divided into thirds, with the target site for injection being the lateral one-third mark. This lies lateral to the femoral nerve and vasculature.
Figure 2. A: In the infrainguinal approach, the fascia lata and fascia iliaca form a “bow tie” when overlapping between the sartorius caudad and internal oblique cephalad, with underlying iliacus muscle spanning over the ilium. B: In the suprainguinal approach, the sartorius overlies the iliacus muscle on its lateral border, with the fascia iliaca separating the two muscles. The femoral nerve and vascular bundle lie medial to the iliacus muscle, and the lateral femoral cutaneous nerve lies between the muscle bodies.
Supplies
- High-frequency linear transducer (6–10 MHz) with sterile lubricant
- 0.5% ropivacaine (5 mg/mL): dilute 30 mL 0.5% ropivacaine into 30 mL 0.9% normal saline
- Max dose is commonly considered 3 mg/kg.
- Ropivacaine is the preferred local anesthetic due to its long-acting duration with a greater safety profile than bupivacaine.13
- Mixing of local anesthetics is not currently advised due to less predictable onset, duration, and potency.13
- 22-gauge blunt-tipped echogenic needle (Whitacre and Sprotte needles are blunt-tipped needles, which provide better tactile feedback when “popping through” the fascia lata and fascia iliaca.)
- IV tubing connected to a 30 or 60 mL syringe
- Chlorhexidine scrub or alcohol prep sponge
- Local anesthetic for cutaneous anesthesia (eg, 12% lidocaine without epinephrine)
- Personal protection equipment including sterile gloves
- Second provider present for assistance
- Airway supplies and 20% lipid emulsion available
With the above supplies prepared and on standby, perform a preprocedure scan to determine the patient’s specific anatomy. Prepare the selected injection site with chlorhexidine or isopropyl alcohol. A skin marker may help maintain proper orientation to the injection site. Next, flush the premixed 30 mL of ropivacaine and normal saline through the line and echogenic needle.
Preprocedural Nerve Block
As with any proximal nerve block, several steps should be addressed prior to beginning the procedure. First, a thorough neurological exam should be performed. Discussion with the orthopedic service at your institution is recommended before US-guided nerve blocks for hip fractures are performed. A detailed lower extremity neurovascular examination must be performed and documented. Patients should be placed on continuous cardiac monitoring and pulse oximetry to monitor for local anesthetic systemic toxicity. The risk of local anesthetic systemic toxicity (both neurological and cardiovascular) is highest in cases of unintentional intravascular injection. In addition to supportive, anti-seizure, and cardiac resuscitation measures, early administration of lipid emulsion antidote is recommended with prolonged seizure and/or any cardiac arrhythmia. Providers should be aware of Intralipid (20% lipid emulsion) availability and dosing prior to injecting large volumes of local anesthetic.14 Lipid emulsion effectively creates a “lipid sink” where the local anesthetic is soluble with, and bound by, the lipid molecules.
Pages: 1 2 3 4 | Single Page





5 Responses to “Control Hip Fracture Pain Without Opioids Using Ultrasound-Guided Fascia Iliaca Compartment Block”
January 27, 2018
Ron BraceThe diagram, first color coded one showing locations of Fem nerve vein and artery is seriously mislabeled and a correction need be done; Femoral Vein is in wrong place, as is the Femoral artery – and the fem artery is mislabeled
I am sure by now a thousand people have written about it!
https://www.acepnow.com/wp-content/uploads/2018/01/ACEP_0118_pg20a.png
January 28, 2018
Robert A.Great article. I think Figure 1 is mislabeled: Femoral artery is mislabeled as “Fem V.” and Femoral vein mislabeled as “Fem N. (red)”.
February 5, 2018
HosamIn illustration, I think that order of structures are not proper.it is vien artery nerve from medial to lateral
February 5, 2018
MikeHi, picture 1 seems to have some errors. There are two structures markes Fem N, one of them in red which is likely supposed to be the Fem Artery. If that structure is supposed to the fem artery it is incorrectly positioned medial to the femoral vein when it should be lateral
February 5, 2018
Dawn Antoline-WangThank you to everyone who pointed out the error in Figure 1. The image has been corrected.