
Hair-Grooming Syncope
When evaluating these patients with low-risk syncope, how often have you asked: “Were you getting your hair groomed when you passed out?”
Explore This Issue
ACEP Now: June 2025 (Digital)Hair-grooming syncope is a rare subtype of neurocardiogenic syncope that is precipitated by different acts of hair care or grooming. Evans, et al., conducted a retrospective study in which they reviewed a database of pediatric patients being evaluated for syncope in the outpatient pediatric cardiology clinic. Hair grooming triggered episodes in seven percent of the cohort—78% of whom were girls. Hair combing was the most common trigger in girls, whereas hair cutting predominated in boys.
Cardiac testing workup demonstrated normal ECGs in 109 of 111 with two patients having minor noncontributory arrhythmias; and 105 of 111 had normal ECG with six patients having minor noncontributory structural abnormalities.2 The authors speculate that the mechanism of hair grooming syncope is related to pain from hair pulling or scalp stimulation of the trigeminal nerve, which precipitates a neurocardiogenic reflex. Although the authors do not specify which branch(es) of the trigeminal nerve are affected, all branches of the trigeminal nerve innervate sensitive areas of the scalp as shown in Image 1.
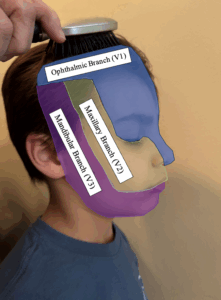
Image 1. All branches of the trigeminal nerve innervate sensitive areas of the scalp. (Click to enlarge.)
Emergency physicians must decide who can be safely discharged with outpatient follow-up (low-risk) and who requires admission for monitoring (high-risk. The next time you see a patient in the emergency department who experienced a syncopal episode when getting their hair combed or cut, you can now potentially “brush” it off as hair grooming syncope.
Teaching Points:
- An ECG should be obtained on all patients who present to the emergency department after a syncopal episode.
- Syncope during hair grooming practices is thought to be a type of neurocardiogenic syncope that occurs because of stimulation of the scalp nerve fibers and/or branches of the trigeminal nerve.
- Although the differential diagnosis for syncope is broad, most causes of syncope are benign, so obtaining a thorough history and performing a physical exam to help identify high-risk syncope are paramount in determining additional workup and disposition.
 Dr. Halupa is an emergency physician at the Geisinger St. Luke’s Hospital in Orwigsburg, Pa.
Dr. Halupa is an emergency physician at the Geisinger St. Luke’s Hospital in Orwigsburg, Pa.
References
- De Lorenzo RA. (2018). Syncope. In Walls R, Hockberger R., Gausche-Hill M, et al. (Eds.), Rosen’s Emergency Medicine: Concepts and Clinical Practice (pp. 115-122). Elsevier.
- Evans WE, Acherman R, Kip K, Restrepo H. Hair-grooming syncope in children. Clinical Pediatrics. 2009; 48(8): 834-836.
Pages: 1 2 3 | Single Page





No Responses to “Case Report: When Syncope Gets Hairy”