
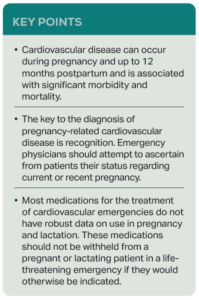
The mortality rate varies by condition, time to presentation, the patient’s access to specialty care, and patient comorbidities. A global registry of peripartum cardiomyopathy (PPCM) reports that fewer than half of patients who experience PPCM will completely recover their left ventricular function.2 The key to making these diagnoses is identifying which patients are at risk. Because the risk for pregnancy-related cardiovascular disease extends many months past the point at which the pregnancy ends, it is recommended that all pregnancy-capable patients be screened for current or recent pregnancy. The most straightforward means to ascertain current or recent pregnancy is for the ED clinician to ask the patient, “Are you pregnant, or have you been pregnant in the last 12 months?”
Explore This Issue
ACEP Now: Jan 01The acute management of cardiovascular disease during pregnancy or in the postpartum period centers on recognizing the condition, supporting oxygenation and ventilation through the provision of supplemental oxygen when necessary, optimizing the patient’s volume status and myocardial function, connecting the patient to timely subspecialty care, and—if necessary—intervening. Many of the medications used in the acute management of cardiovascular emergencies—diuretics, beta blockers, ACE inhibitors, and angiotensin receptor blockers—do not have robust data on their usage during pregnancy or lactation but should not be withheld in life-threatening circumstances. Consultation with cardiology and maternal–fetal medicine specialists is strongly recommended when available.
ACEP and the American College of Obstetricians and Gynecologists (ACOG) together developed an algorithm to assist emergency physicians in the diagnosis and management of patients with pregnancy-related cardiovascular disease.3 The algorithm is shown in Figure 1.
Case Outcome
The patient’s bedside ultrasound was concerning for the presence of three or more B-lines in numerous lung windows, and the patient’s left ventricular ejection fracture appeared globally reduced. The BNP was markedly elevated. ECG revealed normal sinus rhythm with no acute ischemic changes. First high-sensitivity troponin was slightly above reference range. The patient was admitted to an inpatient telemetry bed for continued workup and consultations with cardiology and maternal–fetal medicine due to concern for peripartum cardiomyopathy.
 Dr. White is chair of ACOG’s Obstetric Emergencies in Non-Obstetric Settings Project and an emergency physician at University of New Mexico, Albuquerque, N.M.
Dr. White is chair of ACOG’s Obstetric Emergencies in Non-Obstetric Settings Project and an emergency physician at University of New Mexico, Albuquerque, N.M.
References
- Trost S, Busacker A, Leonard M, et al. Pregnancy-related deaths: data from Maternal Mortality Review Committees in 38 U.S. States, 2020. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services. Published May 28, 2024. Accessed November 22, 2024.
- Hoevelmann J, Engel ME, Muller E, et al. A global perspective on the management and outcomes of peripartum cardiomyopathy: a systematic review and meta-analysis. Eur J Heart Fail. 2022;24(9):1719-1736.
- The American College of Obstetricians and Gynecologists. Identifying and managing obstetric emergencies in nonobstetric settings. Published 2024. Accessed November 10, 2024.
Pages: 1 2 3 | Single Page





No Responses to “Peripartum Cardiovascular Disease Is Rare, But Serious”