The patient symptomatically improved throughout her stay, vitals stabilized, and repeat troponins remained negative. Her leukocytosis and elevated lipase both trended down to within normal values. Her repeat ECG prior to discharge was normal sinus rhythm with resolution of ST changes. She was ultimately discharged on aspirin and atorvastatin, with continuation of apixaban and discontinuation of ticagrelor.
Explore This Issue
ACEP Now: Vol 42 – No 12 – December 2023Discussion
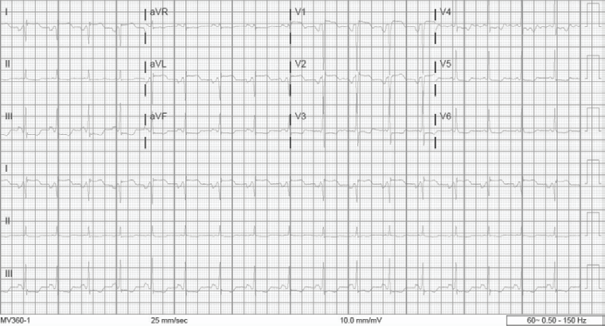
Intra-abdominal etiologies with occurrence of ST-elevation myocardial infarction are rare. With 36 cases involving pancreatic inflammation described in literature, the pathophysiology remains unknown. Interestingly, an inferior wall ST-elevation myocardial infarction has been the most frequent pattern reported.2 Proposed hypothesis as described by Hsu et al., include (1) vagally mediated reflexes, (2) metabolic and electrolyte abnormalities, (3) direct toxic effects of pancreatic enzymes on myocardium, (4) coronary artery vasospasm, (5) hemodynamic instability or systemic inflammatory response, (6) prothrombotic derangement, and others including (7) takotsubo cardiomyopathy.2,4,5,6 In our case, STE in I, aVL and inferior depressions suggested a lateral infarction with a repeat ECG with STE in aVR with diffuse ST-depressions. The patient’s normal electrolytes, catheterization and echocardiogram lead us to suspect the etiology could be related to direct toxic effects, vasospasm or systemic inflammatory response.

FIGURE 3: The patient was taken for left heart catheterization given the dynamic ECG changes in the setting of epigastric pain. Findings were without obstructive lesions and notable only for 20-30 percent stenosis of the left anterior descending artery. An echocardiogram soon after demonstrated a normal left ventricular systolic function with minimal pericardial effusion and no major valvular abnormalities. (Click to enlarge.)
Despite the low frequency, acuity remains high when considering the importance of misdiagnosis leading to invasive treatment and testing. Missing ACS has fatal consequences, as does converting acute pancreatitis to hemorrhagic pancreatitis with thrombolytics.7,8 Catheterization itself carries the complications of dissections, perforations and bleeding. Yu et al.2 describe their patient developing a stroke following PCI, in the setting of pancreatitis induced STE. In the absence of guidelines, a multidisciplinary approach to the clinical situation may be most appropriate. Even still, pseudo-myocardial infarction associated with acute pancreatitis must be a diagnosis of exclusion.9,10 The lethality of true myocardial infarction warrants cardiology consultation for angiography, as opposed to use of thrombolytics.
The presentation serves as another instance where STE signaled systemic disease unrelated to a flow-limiting coronary lesion.11 While our patient’s ECG findings could have represented occlusion, the clinical context proved to be an important factor in avoiding thrombolytics as transport was arranged for angiography. There is both a circumspect and nuanced approach to diagnosing and managing myocardial infarctions. To guide clinical management, the risks and benefits of cardiac interventions must be weighed with factors such as the patient’s stability and likelihood of other diagnoses to make the most appropriate disposition.
Pages: 1 2 3 | Single Page





2 Responses to “Case Report: Pancreatitis Mimics STEMI”
December 31, 2023
Steven VAwesome work! very important to be aware of mimics in this field.
December 24, 2025
JamesThe first EKG shows a limb lead reversal (LA/RA). Lead I is upside down. Leads II and III switch places, and leads aVL and aVR switch places. This is why there appears to be ST elevation in I and aVL. I’m surprised that no one recognized this.