
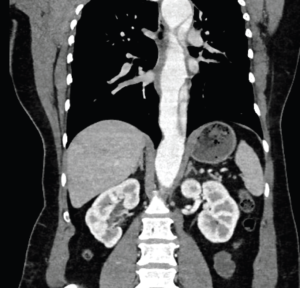
A 40-year-old woman with a history of untreated hypertension presented by ambulance after she was thrown from an ATV at unknown speeds and then crushed by the vehicle. The vehicle had no seatbelt or airbags, she was not helmeted, and she did not hit her head or lose consciousness. She reported 10/10 pain localized to her right arm and right flank, with no other complaints. On arrival, she was stable, airway breathing and circulation were intact, and Glasgow Coma Scale was 15. Initial vitals: HR 90, BP 161/142, RR 24, SpO2 100 percent on room air, afebrile. Primary survey was remarkable for an obvious deformity to the right forearm. Her secondary survey was remarkable for scattered abrasions and moderate bilateral flank tenderness. Her focused assessment with sonography for trauma was negative with bilateral lung sliding. The patient was neurovascularly intact throughout, with right upper extremity motion limited due to pain. Initial anteroposterior (AP) chest radiograph demonstrated no mediastinal widening, tracheal deviation, or pneumothorax. Plain film scout images of right upper extremity demonstrated a midshaft radius fracture.The CT scan of the chest, abdomen, and pelvis revealed a large traumatic Stanford type B aortic dissection. The patient was immediately started on esmolol and nicardipine drips with a systolic pressure goal of 120 mmHg. She was emergently transferred to a Level 1 trauma center by air ambulance, accepted by trauma surgery, and followed closely by vascular surgery.
Explore This Issue
ACEP Now: Vol 43 – No 07 – July 2024This case highlights the importance of recognizing concomitant trauma beyond a distracting injury. Traumatic aortic injury (TAI) is the second most common cause of mortality in non-penetrating traumatic injury; nearly 80 percent of cases die before hospitalization, and, of those who are hospitalized, mortality remains greater than 45 percent, with untreated mortality increasing one percent per hour.3,4 Most individuals suffering TAI are young males injured in motor vehicle accidents or falls.2 Although the most common originating site of a traumatic aortic dissection is distal to the left subclavian artery (LSA), in this case the proximal tear originated immediately upstream from the subclavian and distal to the left carotid artery.2 Plain radiographs of the chest may demonstrate findings of TAI—mediastinal widening, tracheal displacement, abnormal imprints of the aortic arch—but have low sensitivity and specificity, as reflected by normal findings in this case.2 The gold standard for imaging traumatic aortic injury is contrast-enhanced CT, with trans-esophageal echocardiogram being the second-best option if CT is not immediately available.2 Despite the ready availability of trans-thoracic echocardiogram (TTE) and its ability to capture aortic root dilation, cardiac tamponade, and dilation of the descending aorta and abdominal aorta, the sensitivity and specificity of TTE in traumatic aortic injury remains low and should not be relied on.2,3 In this case, aortic dissection was visualized neither on initial bedside nor on repeat inpatient TTE, despite operator knowledge of a known lesion and extensive operator training.
Pages: 1 2 3 | Single Page




No Responses to “Case Report: Imaging Follows Dangerous ATV Accident”