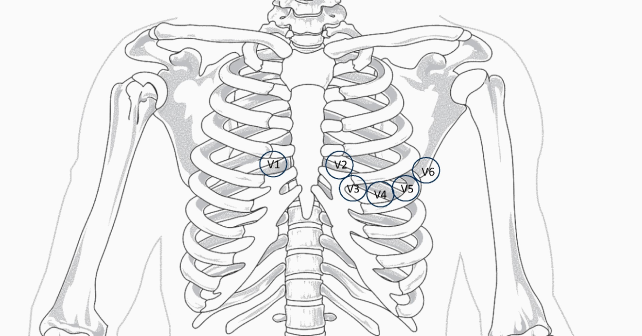
The different morphology of Brugada is shown in Figure 4; although, only type 1 pattern is diagnostic.5,7,8 The ECG patterns of Brugada derive from the conduction delay localized in the right ventricular anterior wall and right ventricular outflow tract. By moving the anterior precordial leads higher on the chest to the second or third intercostal spaces, a Brugada pattern can be brought out (see figure 5).9
Explore This Issue
ACEP Now: Vol 43 – No 10 – October 2024It is estimated that 20 percent of sudden cardiac deaths with a structurally normal heart are attributed to Brugada syndrome.10 The condition is autosomal dominant with variable expression, more common in males, with low prevalence in children (<0.8 percent).7 The ECG findings can be concealed or transient after resuscitation from cardiac arrest. Many cases are asymptomatic, and ECG changes may only be seen intermittently during conditions like fever, vagal stimulation, drug intoxication, or electrolyte imbalances. The absence of findings between episodes makes this diagnosis elusive.
Figure 5: This graphic shows a comparison of traditional and modified location of placement of right precordial leads. (Click to enlarge.)
The most common presenting symptoms are life-threatening arrhythmias, syncope, and cardiac arrest. Diagnosis may be made based on ECG findings and the association of one of the following: documented ventricular fibrillation, polymorphic ventricular tachycardia, family history of Brugada syndrome, sudden unexplained death in family members younger than 45 years old, unexplained syncope or aborted sudden death, as in our case.11 The procainamide challenge test can also be used to unmask latent Brugada syndrome in asymptomatic individuals.12
In children, an ICD is considered a class 1 indication in patients with aborted sudden cardiac death or spontaneous, sustained ventricular tachycardia. Fever and certain drugs can precipitate arrhythmias in this population. A list of medications to avoid in Brugada syndrome are available at https://www.brugadadrugs.org/avoid/. Genetic testing may inform prognosis and management, as certain SCN5A mutations are associated with a higher risk of arrhythmic events; although, the yield of genetic testing is fairly low in this condition.13
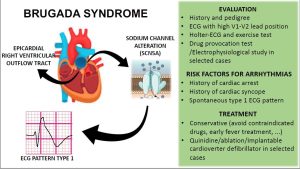
Figure 6: A summary graphic of diagnosis and management of Brugada syndrome in pediatrics. (Click to enlarge.)
A summary approach to diagnosis and management of pediatric patients with suspected Brugada syndrome is shown in Figure 6.
Key Takeaways for Emergency Physicians
- Brugada syndrome is an uncommon cause of sudden cardiac arrest in children. It must be suspected in aborted sudden cardiac death or unexplained syncope in the presence of conduction delay and repolarization abnormalities in precordial leads. It can present as asystole or ventricular fibrillation.
- ECG findings may be concealed or seen intermittently in association with conditions like fever, vagal stimulation or electrolyte imbalances.
- Modified lead placement, with high precordial leads at the second or third intercostal space superior may help confirm diagnosis.
A special thanks to Dr. Elizabeth Sherwin, Pediatric Cardiologist & Electrophysiologist at Children’s National Hospital.
Pages: 1 2 3 | Single Page





No Responses to “Case Report: Cardiac Arrest in a Child’s Structurally Normal Heart”