Abdominal Compartment Syndrome in the Emergency Department
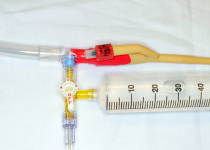
FIGURE 1B
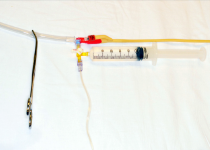
FIGURE 1C
PHOTOS: Michael Gottlieb and Brit Long
Although multiple methods of IAP measurement have been proposed, intravesicular measurement generally preferred. As the name suggests, this measurement is obtained by placing a Foley catheter into the bladder. When measuring IAP, the patient should be supine and relaxed to avoid artificially increasing the IAP measurements.5,10 Ensure the patient’s pain is adequately controlled and measure the pressure at end-expiration.14 Clinicians should use warm saline to avoid detrusor muscle spasm, and no more than 25 mL of fluid should be instilled to avoid false elevations of IAP.14 ACS is defined as an IAP >20 mm Hg with evidence of organ dysfunction.14
Treatment of ACS focuses on improving end-organ perfusion by reducing IAP. This includes four main steps: 1) evacuating intraluminal and intraperitoneal contents, 2) improving abdominal wall compliance, 3) optimizing intravascular fluid therapy, and 4) early surgical consultation for possible surgical decompression.
Ileus and luminal distension are common in patients with ACS.15,16 Nasogastric or orogastric tubes can reduce gastric distension, while prokinetc agents (eg, metoclopramide, erythromycin) may help reduce intraluminal contents.14,17 Extraluminal pathologies (eg, ascites, hemoperitoneum, pneumoperitoneum) may also require drainage, which can be performed percutaneously or through operative drainage.18–20
Adequate analgesia and sedation should be provided because pain and sedation can further increase IAP. If the patient is intubated, clinicians should aim for as low positive end-expiratory pressure and plateau pressures as the oxygen saturation allows.10,16 Paralysis can also be used as a temporary bridge for refractory cases while awaiting surgical decompression.21–23
Clinicians should avoid excessive fluid administration because third spacing will worsen existing ACS.10,16 If patients are hypotensive or septic, early vasopressor and inotropic therapy may be preferable in these patients; norepinephrine and dobutamine have the best literature support in treating ACS-associated hypotension.24–27
In cases that are refractory to the above interventions, surgical decompression may be warranted. Therefore, it is important to consult a surgeon early in the management of suspected ACS patients.
Case Resolution
You suspect ACS and assess the IAP using a Foley catheter. The IAP is 25 mm Hg, and a repeat creatinine level is significantly elevated. You place an orogastric tube, administer metoclopramide, ensure the patient is adequately sedated, and consult a surgeon for possible operative management. The patient is taken to the operating room for surgical decompression.
Pages: 1 2 3 4 | Single Page
Topics: AbdominalAbdominal Compartment Syndrome (ACS)Foley catheterintra-abdominal pressure
Related
-
Case Report: A Pediatric Amputated Juvenile Polyp
January 6, 2026 - 0 Comment -
Case Report: A Male Patient with Iatrogenic Obstruction
October 29, 2024 - 0 Comment -
Why Is This Foley Bag Purple?
May 8, 2024 - 0 Comment






No Responses to “Abdominal Compartment Syndrome in the Emergency Department”