
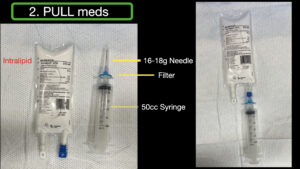
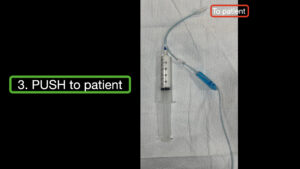
Intralipid solution is readily accessible in our ED, stored in a clearly marked box within the ED block cart and in two automated medication dispensing systems. The ED block cart, which contains all block supplies, including 250 mL of intralipid, is brought to the patient’s bedside for all UGNBs. In conjunction with pharmacy colleagues, we developed a simplified protocol for the administration of intralipid based on the American Society of Regional Anesthesia (ASRA) guidelines, with all supplies and instructions located inside the block cart. The “Open-Pull-Push” technique was created for the initial bolus of intralipid. First, the clinician “opens” the box and removes all the supplies (Figure 1). The clinician then “pulls” a full mL syringe of intralipid through the filter (to reduce large particulate matter) (Figure 2). A 50 mL intralipid “push” is then rapidly administered through the preexisting IV, with this process repeated a second time in rapid succession for a total dose of 100 mL (Figure 3). If the patient remains unstable, this 100 mL bolus can be repeated one more time using the contents of the initial bag.
After administering the initial boluses of intralipid (100 mL, may repeat for a second dose), start the patient on an infusion of 0.25 mL/kg/min. If the patient continues to remain unstable, the infusion can be increased to 0.5 mL/kg/min. In this way, intralipid administration is simplified to a bolus, which is repeated if hemodynamic stability is not achieved, followed by an infusion dose, which is doubled if hemodynamic stability is still not achieved. Once hemodynamic stability is achieved, continue the infusion for at least 15 minutes. The intralipid drip should be made and ready to administer while the clinician is stabilizing the patient with intralipid boluses and ACLS. A laminated information sheet attached to the cart details the ASRA guidelines, which include details on intralipid administration, treatment of seizures, hypotension, and arrhythmias.12 We recommend conducting simulated cases of LAST in the department, so physicians are familiar with the pathway and the equipment.
Summary
Optimal pain control in the ED is a growing field that relies on clinicians learning how to use novel agents (ketamine, nitrous, etc.) as well as UGNBs. With this expansion of knowledge, clinicians must be aware of complications from these novel agents and procedures. For UGNBs, clinicians must be vigilant about patient selection, preparation, and detection of complications. The possibility of LAST should be considered in every case, with proper monitoring and intravenous access. and simple pathways must be in place for antidote delivery. Each ED group should meet with their pharmacy colleagues to ensure there is a clearly defined process for immediate intralipid access and administration during a LAST episode. Stocking our ED block cart with all the supplies to deliver intralipid and our “Open-Pull-Push” technique comes from our desire to ensure all providers have a simplified plan. Aspiration of intralipid through a filter with a large bore needle, and rapid administration should be a learned pathway for all clinicians performing UGNBs in the ED. Like other uncommon procedures, simulated practice will reduce confusion and error in the event of LAST.
Pages: 1 2 3 4 | Single Page






No Responses to “A Simplified Protocol for Intralipid Administration in the Emergency Dept.”