Editor’s Note: This is the third part of an ongoing series on what emergency physicians can do to combat the opioid epidemic. The series will continue in the August issue.
Explore This Issue
ACEP Now: Vol 37 – No 06 – June 2018I feel cheated! After all that time in pharmacology classes and the tests in undergraduate, graduate school, medical school, and residency all oversimplify the concept of the difference between a partial agonist and full agonist. When you dig deep into the pharmacology literature, you find only one true full agonist, DAMGO (ie, [D-Ala2, N-MePhe4, Gly-ol]-enkephalin), which is not even a medication used in humans.
In fact, all the opioid pain medications we give patients are only partial agonists to varying degrees. And as if that wasn’t enough, the ceiling effect of buprenorphine seems to be a myth regarding pain control.
Partial or Full?

Shutterstock.com
As a quick review, we conventionally determine if a medication has partial agonist or full agonist activity based on its intrinsic activity Kappa (Ki). The Ki tells us how much an opioid, or any drug for that matter, activates a receptor when it binds. The strict definition of a full agonist would be any substance that binds to the receptor and activates it 100 percent.
But as stated earlier, there are no clinically available opioids that activate the mu receptor 100 percent. Some get close, such as fentanyl and sufentanil, which activate at about 90 percent. However, others such as hydromorphone and morphine only activate the receptor in the high 80 percent or high 70 percent range, respectively. Buprenorphine effectively reduces the receptor activation to 50 percent. Relatively speaking, opioids have the hierarchy of intrinsic activity shown below in Figure 1.
Why does all of this matter? It matters because buprenorphine is possibly the most important medication in the fight against opioid-use disorder and its close cousin, overdose death. Think about a patient who is physically dependent on opioids, either morphine or hydromorphone. If you give this patient a dose of buprenorphine, you may be called to the bedside and read the riot act because they’re now in acute precipitated withdrawal!

Hailshadow/iStock/Getty Images
It turns out this is not just about the IA of buprenorphine, but also the strength in which buprenorphine binds to the mu receptor, or what’s known as its affinity. For all you molecular biologists out there, we know the receptor affinity data are based on cell culture experiments and mostly in Chinese hamster ovary (CHO) cells at that, not human cells. We therefore must take the absolute numbers of both IA and affinity with a grain of salt.
However, there is a very real clinical issue that comes up when we give buprenorphine to a patient whose mu receptors are inhabited by a more potent opioid that has a lower affinity (see Figure 2).
For example, if I have a patient who’s been on oxycodone and took their last dose right before showing up to the emergency department, and I give them naloxone, this person would go into immediate withdrawal. If I gave that same person a dose of buprenorphine, they would also go into withdrawal. So what’s happening?
Conjure up the image of a dimmer switch on the wall. If we turn it clockwise the light goes up, counterclockwise the light goes down. This brightness of the light is the IA and how tightly we hold the dimmer switch is the affinity. If naloxone is given to a patient dependent on opioids, it is like taking the dimmer switch away from the oxycodone and turning it all the way off, predictably causing acute withdrawal. The mechanism is the same for buprenorphine, but instead of turning that dimmer switch from 85 to 0, it turns it from 85 to 50. Clinically, the end result looks similar, a patient in acute opioid withdrawal.

Dr P. Marazzi/Science Source
This dimmer switch can also work in the opposite direction. If we have a patient who’s physically dependent on opioids and they overdose—that is, they turned the power up so high it kicked off and they caused respiratory arrest—we would give them naloxone. This turns the dimmer switch to 0, allowing the power to come back on.
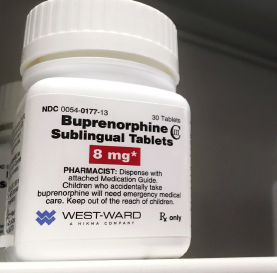
In this all too common situation, we then could follow with a dose of buprenorphine and turn the dimmer up to 50 percent so the patient is no longer in acute withdrawal and still not at risk for respiratory depression. This by itself is pretty cool because now we have a medication we can give 8 mg of sublingually or 0.3 mg of subcutaneously or via IV that will alleviate withdrawal immediately, and we have a patient who is cognitively stable, allowing us to hold a conversation with them about the next steps of their treatment.
Now let me totally blow your minds: What about the patient who’s just overdosed on heroin? If I have no naloxone because I just used it all on the previous carfentanil overdose, could I use buprenorphine?
Theoretically, if there is a low-affinity, high-potency opioid onboard such as heroin causing the overdose, I could give them buprenorphine, a higher-affinity, lower-potency opioid, and instead of causing precipitated withdrawal, it would cause precipitated breathing.
Let’s be clear: I am not telling you to start giving all your opioid overdose patients buprenorphine to wake them up. However, taking into account our newly understood pharmacology, this is a very plausible pathway that would allow a patient to be reversed from respiratory depression caused by heroin with the same medication that would stabilize and treat them.
As we continue to see more and more patients in the emergency department after an opioid overdose, we need to start thinking about issues other than reversal and discharge of these patients. We should be focusing on the stabilization and treatment of these patients, given the high mortality rate of continued utilization of illicit opioids.
It is incumbent upon us to start to use the basic forms of treatment that already exist, are in every hospital pharmacy in the country (or should be), and are a U.S. Food and Drug Administration-approved first-line treatment for this disease. Making a patient suffer from precipitated withdrawal from the naloxone is not teaching them a lesson, it is just mean!
Dr. Waller is a fellow at the National Center for Complex Health and Social Needs and managing partner at Complex Care Consulting LLC.
Send Us Your Questions!
In future articles in this series, we will delineate the best practices for treatment and approach in the emergency department. If you have questions or ideas, feel free to send them our way at schwarze@wustl.edu.
Pages: 1 2 3 4 | Multi-Page






2 Responses to “Buprenorphine Explained, And Opioid Addiction Treatment Tips”
July 18, 2018
Jack McGeachy, MDAs an Emergency Physician with a special interest in the identification and treatment of opioid use disorder among our patients, I was overjoyed to learn that ACEP Now was publishing a series of articles centered around buprenorphine and its potential as a treatment for emergency patients.
I found that this article in particular was concise, yet accurate in its description of buprenorphine’s pharmacology and avoided many of the common misunderstandings surrounding the drug (especially the idea that the naloxone included in Suboxone provides the opioid antagonist property).
However, I believe that it’s critical to correct two misunderstandings that could result in either serious legal trouble or patient harm.
First is the implication of statement that “…we have a medication we can give 8 mg of sublingually or 0.3 mg of subcutaneously or via IV…” which suggests that the formulation of buprenorphine administered is inconsequential. In the context of treating opioid use disorder and acute opioid withdrawal, this is incorrect and it is illegal for a physician to prescribe or administer an opioid drug for these purposes unless that drug carries an FDA approval for the treatment of opioid use disorder.
Although there exist an increasing number of buprenorphine formulations on the market, we are limited to those that are FDA approved specifically for the treatment of addiction, such as Suboxone, Subutex, Zubsolv, Sublocade (implant), or the generics thereof when treating opioid withdrawal and dependency. It would be against federal law to administer a buprenorphine formulation that does not carry this FDA approval such as Buprenex (IM/IV), Butrans (transdermal); even Belbuca, which is a sublingual tablet nearly identical to Subutex, is disallowed for use.
The difference between these groups of medications is that the latter medications are only approved for the treatment of pain, while the former carry an indication for the treatment of opioid use disorder. Unfortunately, this seeming triviality could mean risking a felony conviction for violating the Controlled Substances Act. Institutions have been investigated and fined in the past for their use of injected buprenorphine to treat their patients in opioid withdrawal.
The second troublesome statement is the suggestion is “I could give them buprenorphine…and instead of causing precipitated withdrawal, it would cause precipitated breathing. ” Although the author is trying to illustrate pharmacology rather than give us clinical advice, this implied clinical scenario is implausible. As described previously in the same article, buprenorphine has an extremely high affinity for the mu-receptor. Higher than heroin and even higher than naloxone. You can titrate the dosage of naloxone so that it is bound to enough receptors to reverse the overdose but still leave some receptors available to bind heroin; you can find a happy median between apnea and agony.
In contrast, buprenorphine binds mu-receptors so avidly that it will eventually occupy almost all, leaving no open receptors for heroin to bind. This is the difference between walking down a staircase and jumping out the window; both reduce your altitude, however with the first you can gradually move up or down but once you leave the window, there’s no way back up and only one destination–ground level. Naloxone also has a much shorter half-life, so the agony of precipitated withdrawal is over in about an hour or less. The half-life of buprenorphine is anywhere from 24-48 hours, which ensures ongoing misery for the patient and due its avid binding, there is no way to titrate with another agonist.
This is not to mention the fact that although buprenorphine itself is unlikely to precipitate apnea (due to the “respiratory ceiling” from its partial mu-agonism), it can cause fatal overdoses in combination with other respiratory depressants. Since we often administer naloxone to unconscious patients with no history of their recent drug consumption, it would be dangerous to give buprenorphine to these patients. The patient we assume overdosed on heroin, might have actually taken a few Xanax and the buprenorphine we just administered might very well push them from hypoventilation to full respiratory arrest. Not to mention that the long half life of buprenorphine means that they will be on the ventilator while it is metabolized over days.
I felt it was important to clear up these implied misunderstandings since most Emergency Medicine physicians are unfamiliar with buprenorphine and its applications. I hope that this serves to educate, rather than frighten physicians from adopting buprenorphine in their practice and I look forward to more coverage of emergency addiction management.
July 30, 2018
Evan SchwarzJust to clarify for point 6, it should be dispensed and not prescribed. You do need an x-waiver to prescribe buprenorphine. However, there is a 72 hour rule allowing providers without a waiver to dispense buprenorphine out of the ED for up to 72 hours until the patient can get into follow up. Clearly, this is imperfect as the patient has to come back to the ED for each day to receive the medicine. For patients that are being admitted to the hospital for other issues, the 72 hour rule does not apply and they can be treated as necessary for as long as they are in the hospital. Sorry for the typo but wanted to clarify that. Hopefully one day, all these restrictions will be removed.